Healthcare / Facilities design
Comment
Speech, rest, work, quiet: versatility in healthcare soundscapes
25 Jan 2017 | 0
Healthcare facilities, hospitals, small cities in enclosed spaces; people working, people recovering; babies being born, people dying. Is it really possible to build a place that supports all these different activities? Mai-Britt Beldam explores.
In a recent article, ‘A sound plan: how to achieve optimal healthcare acoustics’, which appeared in the US publication Healthcare Design, writer Barbara Horwitz-Bennett highlighted how since 2007, noise has been the lowest-scoring category in the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. It’s a disappointing finding, especially when one considers recent advances in building materials and improved acoustic design knowledge among designers. Is noise, then, really a problem in healthcare facilities, and, if so, where are we failing?
It's all about the people
As a starting point, let’s look at the end-users who complain. The patient is already out of his or her comfort zone when entering the hospital, firstly, because he or she is sick and, secondly, because he or she knows that when someone is admitted to a hospital, something is wrong. This condition alone will sharpen your senses, because the ‘caveman’ instinct within all of us is to survive.
Human hearing is constantly alert – night and day – especially when we’re sick, stressed or in an unfamiliar environment, and we react to new patterns in the soundscape. A beeping alarm will increase the body’s cortisol levels; a doctor’s footsteps along the corridor can cause a momentary pause in breathing, owing to the fear of potential bad news; and constant background noise is challenging for sleep and recovery. 
In 2010, CH Wiese concluded that high sound levels in healthcare facilities are known to: impair sleep; increase stress; delay post-illness rehabilitation; aggravate agitation; cause psychiatric symptoms; escalate restlessness; increase respiratory rates; and increase heart rates.1 So when patients complain about noise, it’s clear it needs to be addressed.
On the other hand, for the working staff, who are not out of their comfort zone while at hospital, one of their hardest tasks is communication. A doctor, for example, might judge a patient who has just undergone heart surgery to be in their best state of health for, say, 20 years; but the patient might reasonably assess that they had just experienced a heart operation, and were therefore not in particularly good health. Speech and communication are crucial, and to ensure that the intended listener receives the right message, staff members need soundscapes that are conducive to clarity of speech.
It’s stressful when you feel that you’re not understood and, in a lot of cases, bad acoustics and poor quality of speech lead to mistakes. In the US, the Joint Commission’s ‘Sentinel event data’ (‘Root causes by event type’, 2010) shows that 70% of critical medical errors in emergency departments can be traced to “communication shortcomings”, such as multitasking and interruptions. At the same time, healthcare staff have the same sensory system as patients so, of course, they too will be affected by noisy alarms, high levels of background noise, and lack of tranquility. In an emergency situation, when a staff member is fully focused on a patient, they don’t feel noise as a stressor and don’t feel affected. But, as Mahmood et al point out, the body and brain will unconsciously react, and fatigue, stress and tiredness will often follow.2
What can be done?
The first question to ask before trying to address noise issues in hospitals is why we should do anything at all. It’s tricky to attach a figure to a communication error or a doctor’s state of tiredness – and even though everybody in healthcare knows that patient rest and recovery are crucial, these are also hard to put a value on. Whether we like it or not, we always need to discuss prices and costs; but the positive news is that it is indeed possible to calculate the financial contribution of a good acoustic environment.
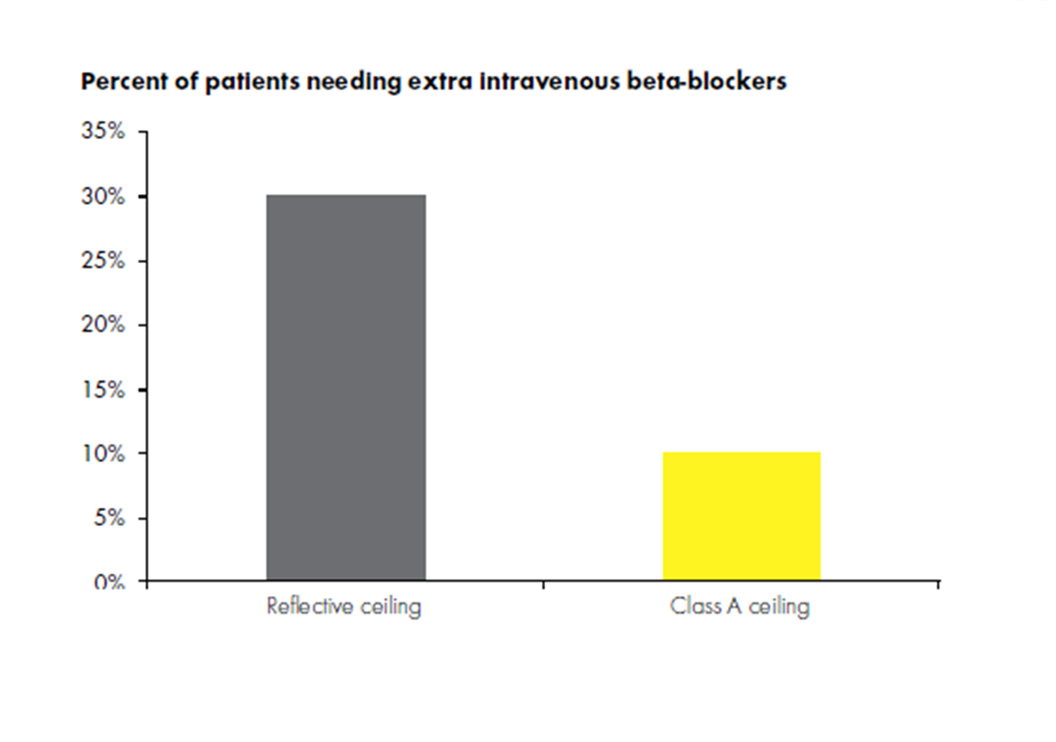 Research has shown correlations between room acoustics, noise levels and medicine intake. In 2005, Hagerman et al investigated what happened to patients with chest pain when the room acoustic conditions are changed.3 The study took place over eight weeks; for the first four weeks the ceiling of the room used was a reflective type, while for the remaining weeks, the ceiling consisted of class A sound absorbers (sound absorbers are classified from A to E, where A is best). The researchers found that during the period when the group experienced poorer acoustics, there was a significant rise in the need for extra intravenous beta-blockers. They also found that during the four-week period when the better acoustics were experienced, the group considered the attitudes of staff to be much better. While it’s possible to attribute a price to the difference in medical intake, it’s far harder to attach a cost to a time when a patient finds a doctor’s attitude to be lacking.
Research has shown correlations between room acoustics, noise levels and medicine intake. In 2005, Hagerman et al investigated what happened to patients with chest pain when the room acoustic conditions are changed.3 The study took place over eight weeks; for the first four weeks the ceiling of the room used was a reflective type, while for the remaining weeks, the ceiling consisted of class A sound absorbers (sound absorbers are classified from A to E, where A is best). The researchers found that during the period when the group experienced poorer acoustics, there was a significant rise in the need for extra intravenous beta-blockers. They also found that during the four-week period when the better acoustics were experienced, the group considered the attitudes of staff to be much better. While it’s possible to attribute a price to the difference in medical intake, it’s far harder to attach a cost to a time when a patient finds a doctor’s attitude to be lacking.
More than absorption
There is no doubt that good room acoustics with absorbent ceilings and wall panels are crucial for a healthy recovery and healthy working environments, but absorption of sound doesn’t solve problems alone. Equally important is sound insulation.
Adjacent rooms should be built to avoid sound transmission from one room to another and the design of a hospital should support ‘acoustic behaviour’. The fridge and other noise-producing equipment, for example, shouldn’t be located in the corridor – not only because of the noise such equipment generates but also because of the unnecessary traffic in the corridor that their presence is likely to attract.
Why do alarms have to be so loud, when research shows that hospital alarms can be softer than background noise levels without staff performance levels dropping?4 Why not talk to the patients about whether they would prefer single bedrooms or multi-bed arrangements? An extrovert would probably find it calming to have someone to talk to, in comparison to an introvert, who might find recovery more challenging if he or she had to share space with another person. Psychoacoustics could be a worthwhile consideration n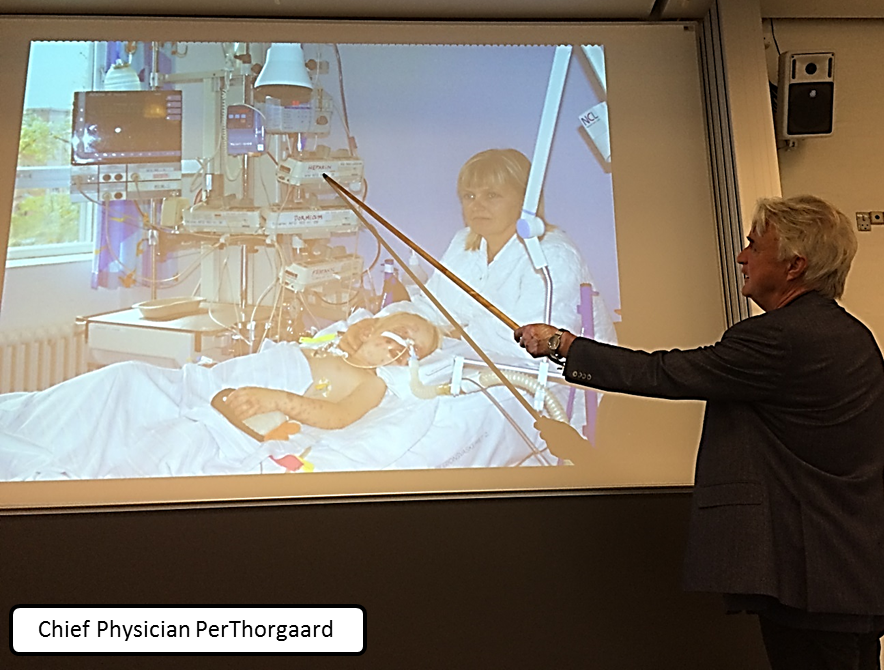 ot only for patients but also for staff. Resources will, of course, come into play, but the biggest thing that can go wrong is if noise, acoustics and sound issues are only addressed after a healthcare facility has been built, rather than during the design phase itself.
ot only for patients but also for staff. Resources will, of course, come into play, but the biggest thing that can go wrong is if noise, acoustics and sound issues are only addressed after a healthcare facility has been built, rather than during the design phase itself.
At a meeting of the Danish Acoustical Society last autumn, Danish chief physician and anesthetic specialist Per Thorgaard opened his presentation with these words: “Patients don’t recover at the hospital. They do that at home, so get them well enough to get them home!”
Which takes us back to the soundscapes of healthcare facilities. These must support the range of distinct user activities that take place in hospitals: ie the essentials of speech, rest, work and quiet. All can be catered for – but it demands different specialists from different fields in the process to come together during the design phase and map out what is most important, and discuss how to create a positive sound effect on people.
References
- Wiese, CH. Investigation of patient perception of hospital noise and sound level measurements: before, during and after renovations of a hospital wing. Architectural engineering – Dissertations and Student Research. University of Nebraska, Lincoln, Digital Commons. 2010; Paper 4: p7.
- Mahmood, A et al. Nurses’ perception of how physical environment affects medication errors in acute care settings. Applied Nursing Research. 2011; vol. 24, issue 4: pp229–237.
- Hagerman, I et al. Influence of intensive coronary care acoustics on the quality of care and physiological state of patients. International Journal of Cardiology. February 2005; 98(2): pp267–270.
- ‘Is it safe to turn down the volume of hospital alarms? New study chimes in: ‘yes’’. Anesthesiology News. 6 December, 2016; www.anesthesiologynews.com
Organisations involved

