Healthcare / Service redesign
Critical care design of tomorrow: how technology fits in
By Diana Anderson and Neil Halpern | 16 Aug 2016 | 0
The future ICU will require a robust life-support system capable of organising information and creating a connectivity envelope around the patient, interfacing with the ICU and hospital networks. A deep understanding of advanced informatics within the ICU and use of new technologies will therefore be vital to the future of ICU design, as this paper explains.
Authors of scientific paper:
Abstract
Advances in networking and remote monitoring capabilities have already begun to redefine the physical and organisational boundaries of the intensive-care unit (ICU). Although commonly thought of as a self-contained unit, the ICU draws on informatics resources located outside the physical space of the unit.
Purpose
The primary objective of deploying advanced informatics within the modern ICU is to electronically integrate the patient and all aspects of patient care with hospital and ICU-based informatics systems. The second goal is to transform all patient-related data into actionable information using smart technologies. This paper will explore both the operational and design requirements needed to ensure this connectivity envelope.
Methods
Upcoming technologies are changing the interface of care collaboration and patient monitoring, requiring ICU design strategies that can incorporate them. These issues will be explored through the perspectives and experiences of two experts – an intensivist practicing critical-care medicine and a healthcare architect trained in internal medicine. Accounts of advanced informatics and technology within the critical-care environment will be discussed in the form of case studies, existing design guidelines and project examples.
Results
The smart ICU infrastructure necessitates the development of a connectivity envelope, which encompasses the patient, medical devices, healthcare staff, and pharmacologic and other care elements. This requires the integration of bedside wired and wireless infrastructure, connectivity hardware within the patient room, medical devices to transmit their data, and the placement of middleware (the software that connects medical devices with the hospital’s operating systems) on hospital and ICU networks.
Real-time locating solutions can improve management and workflow by tracking or locating tagged assets, monitoring device utilisation and controlling product inventory. Devices can be monitored by middleware, thereby supporting web-based device viewing, alarm transmission and remote troubleshooting.
New informatics systems help transform data into actionable information, highlight the most important patient alarms, and enhance infection control and patient room management. This evolution of technology may also focus on bridging the gap between limited numbers of staff and a growing critical-care patient population.
Conclusions/Implications
The ICU of the future will require a robust life-support system capable of organising information and creating a connectivity envelope around the patient, which interfaces with the ICU and the overall hospital networks. An in-depth understanding of advanced informatics and the use of upcoming technologies in the practice of critical care are vital for the future of ICU design.
Keywords
In 2010, there were approximately 6100 intensive-care units (ICUs) with more than 104,000 beds in the 3100 acute-care hospitals in the United States.1 Periodically, these ICUs need to be renovated or new ICUs built. The roles of ICU design and the design teams are paramount when considering the overall process of critical-care design.2 An equally important component that becomes highly relevant for the future is the integration of advanced ICU informatics into the design process. This includes the conceptualisation, actualisation, use and maintenance of medical technology advances.
Part I of this manuscript will review key concepts in current ICU design practice;3 part II will introduce the notion of the ‘smart ICU’ and the steps involved in designing an ICU that electronically integrates the patient with all aspects of care.4
Several core principles should guide ICU specific design, including the following:
- the ICU can be considered a semi-autonomous mini-hospital;
- the unit should be harmonised with other ICUs and hospital support services;
- design innovation must balance functionality, space and physical limitations, cost, security, and healing;
- long-term functionality for a decade or more needs to be considered;
- ICU design should embrace evidence-based design (EBD),5,6 where design decisions about the built environment are predicated on credible research to achieve the best possible results in positive healthcare outcomes, workforce safety, staff satisfaction and productivity, cost savings, and energy efficiency;7–9 and
- the smart ICU employing advanced informatics should comprehensively and electronically integrate the patient into the ICU, with respect to all aspects of care, transforming patient-related data into actionable information using ‘smart’ or ‘intelligent’ technologies.4
Part I: the ICU design process
As critical care is multidisciplinary, the ICU design process benefits from being inclusive and collaborative.2,7 Therefore, the ICU design team should consist of a variety of disciplines including hospital administration, the ICU clinicians (physicians, nurses and pharmacists), allied healthcare support (infection-control specialists, respiratory therapists), and the technical groups (architects, engineers, equipment and informatics). It is also important to include end users (patient and family representatives), as these groups offer different insights.8
Two primary sources guide this team in their design process: the ‘Guidelines for Design and Construction of Hospitals and Outpatient Facilities’,10 published by the Facility Guidelines Institute (FGI); and the ‘Guidelines for Intensive Care Unit Design’, published by the Society of Critical Care Medicine (SCCM).11 The FGI focuses on minimum standards for design and construction (space, risk assessment, architectural detail, surface and furnishing needs, and engineering). The SCCM guidelines describe universal functions that should be accommodated in the modern ICU. Both publications have expanded their recommendations to include the social, psychological and/or cultural aspects of facility performance, addressing the need to comprehensively approach the ‘softer’ aspects of health facility design. The SCCM also maintains a digest of the ICU design award winners and includes architectural design drawings, pictures and videos of outstanding ICUs all over the world.12
ICU layout
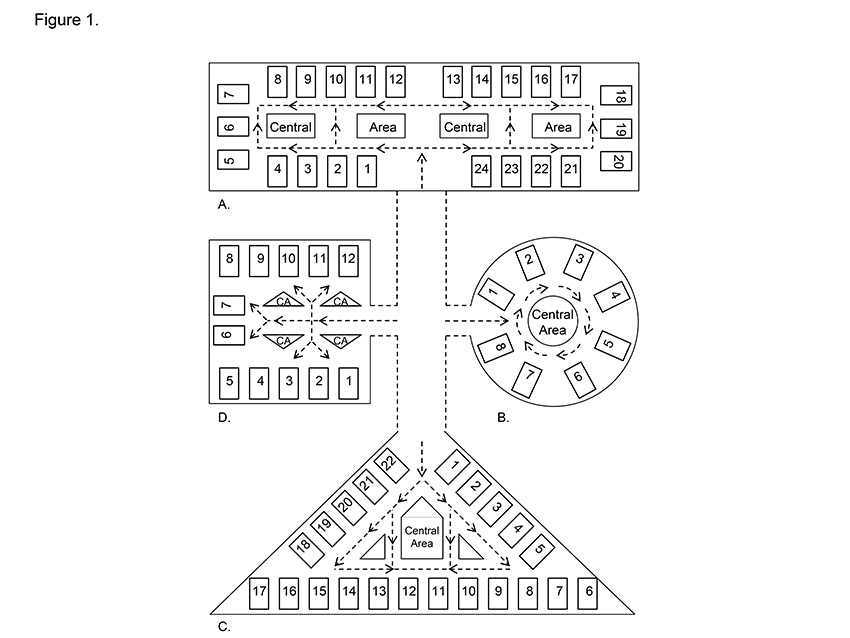
The ICU layout is arguably the most important design feature that affects all aspects of intensive-care services (patient privacy, comfort and safety, staff working conditions, throughput, circulation, logistical support and family integration).13 Layout also influences the location, relation and functionalities of different spaces within an ICU. Depending on the physical limitations of the space, designers have applied various types and combinations of layouts (see Figure 1).14 The racetrack (patient beds around the perimeter with services in the centre and a loop corridor space in between) appears to be the most dominant unit layout among award-winning adult ICUs.
ICU patient room
The central point of the ICU experience is the patient room.3,5,11,15 Guidelines advise use of single-bed10,11 rather than multi-bed rooms, in order to enhance patient safety, privacy and infection prevention. Each room should be equipped to function as an autonomous area with the necessary space for caregivers, procedures and visitors,16 and should offer a healing environment with access to outdoor views through windows. Concomitantly, the rooms should be fully interwoven into the ICU, hospital workflow and social fabric. Ideally, all ICU patient rooms should be standardised for layout. The patient rooms can be designed identically (same-handed) or as mirror images of each other.17 Room standardisation may save design and construction time, as well as improve patient safety.15,18 Importantly, patient room standardisation allows staff to move in and out of each room efficiently because the staff always know where devices are installed and supplies stored. Additionally, patient rooms should be standardised according to the minimal size requirements in FGI guidance and state-based rules.10
ICU patient rooms can be subdivided, physically or virtually, into four zones: patient, caregiver (work), family (visitor) and entry way (see Figure 2).3,11 The room’s focal point is the patient bed. Optimally, all supportive infrastructure services (medical devices, gases, vacuum, plumbing, electrical and data jacks, communications and entertainment systems) should be installed on a medical utility distribution system – clearing the floor and facilitating ready access to the patient by visitors and staff.19 There is a choice between fixed (wall or floor) mounted headwalls or columns, and mobile articulating columns (booms) mounted to ceilings or walls. Stationary systems are less expensive than mobile systems, but mobile booms offer greater flexibility, patient access and bed movement.
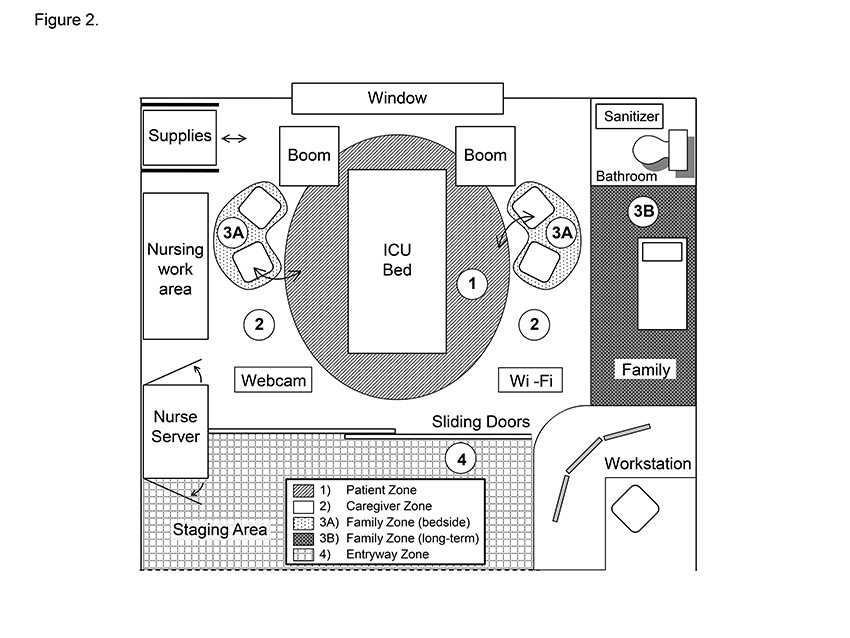
The caregiver zone includes work areas and space for medication preparation and procedures, as well as computers, displays and storage areas. The design of the caregiver physical environment should not hinder the interplay between critically ill patients and their families. The family zone should incorporate amenities such as comfortable chairs, power outlets, wireless access and, if space permits, a long-term visiting alcove. The entry way of each patient room may open directly out to the hallway or be set back. Opening directly out to the corridor provides the largest possible patient room, but setting the room back may provide a staging area that incorporates a decentralised workstation, handwashing system, storage space, coat hangers, and identification and informational display systems. A hybrid design that incorporates both direct hallway access and a set-back may provide the best of both worlds.
Core ICU-room medical devices should ideally include: the ICU bed; physiologic monitor; mechanical ventilator; infusion and feeding pumps; pneumatic compression devices; patient lift; computers; chairs for patient and visitors; over-bed tables; laboratory-specimen label printer; nurse-call intercom station; webcam; entertainment system; storage areas; and waste disposal bins. The design team should also address point-of-care testing (POCT) and ultrasonography, and whether these devices should be placed in each room or positioned centrally. Adequate storage spaces for supplies, medications, linens and waste management systems should be incorporated into each patient room. Nurse servers (cabinets with bi-directional and secure access from both outside and inside the room) may be a good solution to improve privacy and infection control, by stocking the room from the outside.
ICU patient rooms must now have direct access to separate enclosed bathrooms.10 The design must therefore determine the optimal bathroom location (ie front of room, back of room, or front and back of adjacent rooms). These decisions are likely based on the availability of plumbing; nevertheless, the impact on patient visualisation, window availability, or workflow is quite important. Patient bathrooms should have either sanitisers to clean reusable bedpans or macerators to destroy single-use bed pans.
Decentralised workstations
The front of the ICU patient room is the interface of the room with the ICU hallway and ICU central areas. This space controls room entry, patient privacy, sound transmission, infection control, impedance of smoke, and allows for patient observation and monitoring. Options for front-of-room privacy include curtains alone, curtains behind clear glass doors, and glass doors with integrated privacy solutions (manually or electronically controlled integral blinds or electronic glass (LCD or e-glass). Curtains are more economical to install than glass systems, but curtains are not effective controllers of sound, infection or smoke. Glass systems are also easier to clean.
The front of each room provides a ready location for patient observation and monitoring through incorporation of a clinical decentralised workstation. These workstations facilitate the deployment of staff close to the patient and there is usually one for every room or every two rooms, depending on space considerations and room build. The workstations should have ready digital access to all bedside physiologic data (mirrored on displays or web-based) and the electronic medical record.
A healing environment
Although the exact design features that transform ICUs into healing environments are not definitively identified, it is well known that the physical environment affects the physiology, psychology and social behaviours of all those who experience it.6,20 Therefore, it is imperative that the patient-room environment promotes healing and serenity by addressing sound, light, temperature, visuals and entertainment.21
Sound control positively influences patient outcomes by lowering physiological stress, sleep disturbance and feelings of fear.22 The highest noise levels in the ICU have been shown to be related to staff conversation and the use of advanced technical equipment. Acoustic control in the ICU is generally achieved through the integration of sound minimisers (sound-absorbent finishings and ceiling tiles, acoustic baffling in the walls, sound-resistant windows, and sound attenuators in the HVAC system), patient-level sound mitigaters (sound-cancelling headphones or sound masking) and systems that control alarms and communication broadcasts.
Natural light is also essential to the wellbeing of patients and staff, and ICU patient rooms are now required to have windows.10,11,21 The glare associated with windows, however, should be controlled by installing anti-glare glass and light-reducing shades. The room itself should have multiple lighting arrangements to accommodate changing times of the day, physical examination, and procedural requirements.
Another element of healing is artwork – this can be permanent and mounted on the ICU walls, embedded in privacy curtains and ceiling tiles, or electronic and projected on video displays, televisions or computer screens, or directly through visor-based video displays. A ‘low-tech’ white board should also be available in each room for the display of positive messages, get-well cards and family pictures.
Electronic and computer-based integration of the environmental (light, shade, temperature, artwork) and entertainment systems with remote handsets (pillow speaker) or wall-based computer switches supports efficient patient and staff-centred control of the room. Environmental profiles can then be tailored to particular needs (day and night, procedures, and patient needs). Multi-parameter sensors that monitor temperature, humidity, light and sound, and provide alerts for uncomfortable environmental circumstances, also help track and maintain the healing environment.
Central care stations
The central stations and corridors unite all the patient rooms, as well as other supportive areas, and create unit cohesiveness. The goals of all central areas are to support bedside care, offer a welcoming and warm atmosphere, and provide access to logistical support areas. Design of these areas is governed by the hospital and ICU approaches to centralised or decentralised care, logistics, and space availability.
The composition of the central care stations includes greeting desks, areas for quiet work and conferencing, as well as offices and restrooms. Technologies usually include nurse-call communication stations, telephones, computers, high-definition image review stations, laboratory-specimen label printers, pneumatic tube stations, nourishment stations, emergency alerts, and cut-off switches for ICU utilities.
In a small ICU, one centrally located station may suffice; in contrast, multiple central stations may be needed in a large ICU with several bed pods. The layout of these areas is primarily affected by bed configurations. Optimally, unobstructed views of the ICU beds should be available from the central care stations. Studies have suggested that decreased visibility may negatively affect clinical outcomes for severely ill patients assigned to rooms that offer poor visibility.23,24 Because unimpeded views are commonly precluded by the ICU layout, visibility from central areas can be enhanced electronically through the use of webcams in each room and central displays of bedside devices.
Corridors
ICU corridors provide pathways for transit and promote physical and social unity. If possible, separate designated hallways for patients and supplies augment patient privacy and decrease visitor distractions. Corridor design may also have to support access to imaging and procedural suites, and provide passage for very large mobile imaging technologies (eg mobile CT scanners). The corridors, through their finishings, artwork, sound control and lighting, set the emotional tone for the ICU. These considerations are relevant, as hallways are commonly used to conduct rounds, impromptu clinical consultations and family meetings. Moreover, corridors may impact the patient psyche, as patients frequently walk along them as part of their early mobility programmes.25
ICU storage
The correct sizing and proper positioning of the storage areas (central and bedside) requires a sound understanding of the logistical approaches (centralised and/or decentralised) that the hospital and ICU deploy. Appropriately allocating storage space also requires correct assumptions of ICU supply utilisation of consumables. Outfitting storage units and expensive supplies and equipment with electronic tags promotes inventory management, and permits the use of real-time locating systems/solutions (RTLS).26 Storage spaces may include traditional supply rooms, as well as alcoves along the ICU hallways. Storage spaces should be accessible to transport or cargo elevators and be fairly close to patient-care areas. Central storage spaces must also be able to handle and charge supplementary medical devices (eg infusion pumps, ventilators, and specialty monitoring or imaging devices).
Pharmacy, ICU laboratory and POCT
Hospitals may have centralised or decentralised pharmacy and medication distribution systems and staffing models. Therefore, ICU pharmacy systems must be coordinated with the hospital’s pharmacy and ICU bedsides. Options include a fully equipped satellite ICU pharmacy or a pharmacy area with minimal resources. Both alternatives commonly utilise decentralised self-contained and secure automated medication-disposing units. Medications may also be stored in secured cabinets at the ICU bedside.
Many ICUs utilise laboratory testing from a centralised lab. If point-of-care testing is incorporated, however, the design must accommodate POCT systems.27 A combination of POCT modalities and locations may be used, depending on the ICU workflow, required testing, and available space and resources. Pneumatic tube stations are still required to transport specimens to laboratories outside the ICU area, as POCT is never a complete replacement for the central laboratory.
Infection control and prevention
Effective infection control requires an ICU culture that is responsive to infection deterrence, and an ICU infrastructure designed for infection prevention. Core infrastructure elements include systems that provide clean air and water, and waste sequestration and elimination. Non-porous, well-sealed and easy-to-clean surfaces and finishings throughout the patient rooms, and ubiquitous, visible and accessible hand sanitisers and fluid dispensers are critical to infection control. Advanced modalities include electronic handwashing surveillance, self-cleaning copper or silver surfaces, surface surveillance monitors, and the use of environmental decontamination systems (eg ultraviolet light, hydrogen peroxide dispersion, and continuous air disinfection).3
Wayfinding, visitor and staff support
In addition to a well-designed ICU layout, good signage is necessary for efficient wayfinding. Directional signs should be clear in their message and easily visible. Destination signs should identify each room, with signs at the ICU entrance providing information about the unit and, potentially, including its designation (eg surgical ICU), management names (eg ICU director and nurse leader), and visiting hours.
Family support is a significant factor in emotionally sustaining the ICU patient. Concomitantly, family members become emotionally depleted when their loved one is an ICU patient. With these factors in mind, it is important to build family ‘waiting’ areas to promote visitor wellness.28 The waiting areas should have soft lighting, quiet background music, warm colours, large windows, nature-themed artwork, and be in close proximity to the ICU to allow visitors to recharge between visits with their loved ones. Privacy, nourishment areas, bathrooms, lockers and coat hangers should be provided. Informatics support may include wireless Internet access, computers, and smartphone charging stations. Long-term sleeping accommodation, if possible, provides space for visitors who prefer to remain nearby. Inclusion of consultation rooms and social work offices also helps promote family meetings and social support.
Similar to ICU visitors, clinicians working in ICUs regularly face extreme stress. Therefore, the ICU design must address the impact of staff spaces. Well-designed staff lounges (break rooms) and on-call suites located within the ICU provide a place adjacent to patient care for staff to relax. Lounges should have windows to the exterior, comfortable seating and tables, as well as access to computers, ICU communications and entertainment. Bathrooms, changing areas, lockers and scrub dispensers, napping alcoves, and nourishing stations complete the lounge furnishings. In ICUs that maintain clinician availability 24/7, sleeping accommodation (on-call suites) with bathrooms and showers should also be provided. Staff meetings, educational programmes and family meetings are sustained through the construction of multi-purpose conference rooms in the ICU environment. Furnishings should include comfortable seating, conference tables with built-in informatics access, audio-visual-video systems, wireless access, smart boards, electronic attendance and scheduling systems, and food preparation and storage areas.
Part II: Advanced informatics within the ICU
The deployment of advanced informatics into an ICU, thus creating a ‘smart’ ICU, provides enormous positive potential for unit operations.4 Designing the informatics infrastructure, however, requires a different skill set than the standard build, and therefore, requires a team trained in the intricacies of informatics. The main objective of advanced informatics systems should be to integrate electronically the patient and staff with all aspects of care. The second goal is to transform all patient-related data into actionable information. The biggest challenges in this endeavour are harmonising the technologies of multiple vendors into an operational platform that will meet the ICU needs and be fully synchronised with hospital informatics systems.
Building the smart ICU: five steps
The smart ICU infrastructure requires a connectivity envelope around the patient (Figure 3). This envelope encompasses the patient, medical devices, healthcare staff, as well as pharmacologic and other care elements.4
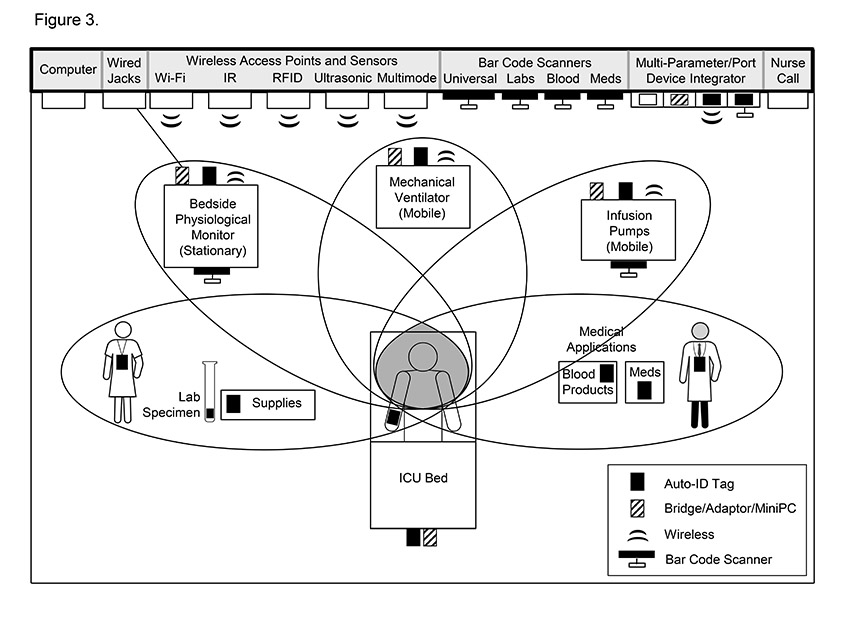
The first step in this five-step process is the installation, within the ICU, of a robust wired and wireless infrastructure that is fully integrated with the larger hospital network. The second step is the placement of connectivity hardware in each patient room to communicate with all data sources. The third step involves the placement of automatic identification (Auto-ID) tags on all data sources for tracking purposes. These tags convey source identification data to a real-time locating system (RTLS). The fourth step is the attachment of adaptors and computers to various medical devices, in order to transmit data and initiate interoperability protocols between medical devices and receiving systems. Finally, the addition of middleware (the software that provides interoperability and other applications between medical devices and the hospital’s operating systems) to both the hospital and ICU networks is needed.4
ICU middleware
The FDA classifies middleware as either Class 1 medical device data systems (MDDS) or Class 2 devices. MDDS devices maintain data storage and transfer, and also convert proprietary device languages into interoperability-standardised formats. Additionally, Class 2 applications offer active patient monitoring and alarms, and therefore receive enhanced FDA scrutiny. Applications inherent in ICU middleware include:
- transforming hospital and ICU data and alarms into actionable information;
- managing devices, applying real-time locating systems;
- creating smart displays, providing decision support; and
- facilitating telemedicine programmes.
The hospital’s bed management system should be interfaced with the ICU middleware to automatically populate or depopulate the middleware with patients as they are admitted or discharged from the ICU. The middleware should also be compliant with hospital privacy protocols and have off-site back-up systems.
Advanced ICU informatics concepts
Integral to advanced informatics are four concepts: association; interoperability; time synchronisation; and medical devices as informatics platforms.
The first concept is the association or linkage (location or patient centric) of the patient with the medical devices and the data generated by those devices (Figure 3). The location-centric approach uses the patient’s location for data linkage while the patient-centric approach uses the patient’s unique medical record number. The location-centric solution is simpler to implement than the patient-centric method, however, the latter solution always attaches the data to the patient regardless of patient movement in the hospital.
The second concept is the application of interoperability between systems. Interoperability aligns the proprietary data output languages of the medical devices with the recipient middleware. Interoperability allows the data generated by one device to be clearly understood by the receiving middleware. Without interoperability, the data produced by the medical device may not be integrated into the electronic medical record, even though the devices are connected to the hospital network.
The third concept addresses time synchronisation between all medical devices, middleware and the hospital network. Time synchronisation helps create a correctly time-stamped medical record for data from all sources, including the tracking of alarms and responses. This can be challenging to attain given each device has its own internal clock, and disparities between devices and systems may be exacerbated when data are transmitted across the multiple components that together comprise the hospital network.
The fourth concept equates medical devices with informatics platforms. All new medical devices can be considered advanced computers, with consistently changing software versions and occasional hardware upgrades. Informatics purchases should, therefore, be carefully assessed in simulation laboratories to evaluate best their proposed informatics capabilities. In all informatics platforms, the costs of annual software upgrades and licensing agreements should be budgeted prospectively. Infusion devices, for example, are now infusion platforms, which include channels, device brains, drug libraries, medication-dosing protection algorithms, connectivity hardware and software, and device management middleware. These sophisticated systems require multidisciplinary coordination.4
Alarm systems
Alarm middleware transforms alarms from medical devices into relevant and actionable information. Such middleware can deliver select alarms to designated providers in real time, in a variety of formats and displays. The most sophisticated of these systems can process and create customised alarms based on combinations of alarms and other data (eg multiple physiological and laboratory values), as well as create personalised patient alarms from streaming raw device data.
Virtual device communities
Standalone medical devices (eg mechanical ventilators) are commonly linked to an individual patient. Alternatively, all ventilators can be linked through device middleware to generate a ‘virtual’ ventilator (device) community. In this setting, one can view all ventilators (settings, data and alarms) in the facility simultaneously. Additionally, such systems provide data storage, alarm transmission, report generation, remote viewing capabilities, and a portal for software upgrades and device monitoring by the vendor.
Real-time locating systems (RTLS)
RTLS middleware offers solutions to improve workflow efficiencies of all assets (staff, patients, equipment, consumables and patient rooms).26 To date, RTLS are used primarily to locate tagged devices (mobile asset tracking) and to provide notification if devices leave designated areas. RTLS can also track the usage of consumable-tagged supplies to monitor inventory and directly link supplies to patient utilisation. Within the ICU, RTLS can be integrated into nurse-call systems and used to monitor patient and staff movements, as well as compliance with handwashing protocols, and the environment.
Data integration, smart displays and decision support
Middleware applications can integrate, transmit and display data from a host of sources (eg EMR, bedside devices, bed management systems, RTLS, imaging servers, webcams, and decision-support systems). Such data can then be displayed imaginatively in a variety of formats and devices. Other middleware systems provide real-time intelligent algorithms and decisions-support, in order to monitor and ‘sniff’ (automated systems that search for pre-selected data elements) for clinical abnormalities that may be invisible to traditional monitoring.
Communications
Telephones, smart phones, nurse-call intercom systems, pagers, and bi-directional transmitters are integral to the ICU communications environment. These devices may all be integrated into one platform (eg within a nurse-call system, a primary communication platform or an alarm system). Functionalities include point-to-point and global messaging, telephone and alarm communications, and real-time locating of staff. Even in these advanced settings, landline telephones and overhead speakers continue to be of value in providing reliable ICU communications. In addition to pre-set panic alerts on handheld communication devices, the installation of panic buttons is suggested in commonly used work areas, in order to ensure staff safety.
Telemedicine
The ICU informatics design also provides the framework for telemedicine through the use of interfaces and bi-directional communications systems. These technologies transmit data, clinician orders, video and voice between the various ICU areas and the telemedicine vendor’s bunker, and access telemedicine support systems. Such solutions are applicable whether the hospital outsources telemedicine to a third party at either an on-site or off-site location, or internally to the hospital’s own telemedicine team. Alternatively, the hospital can install web-based middleware that interfaces with hospital systems and allows the critical-care team to review all hospital and ICU systems, as well as various handheld platforms.
Maintaining the advanced informatics environment
Ongoing maintenance needs of the smart ICU are extensive and should be addressed early in the design process. This type of support requires close collaboration between the design team, and the informatics and biomedical engineering groups, in addition to the development of protocols for continuous monitoring of middleware systems. Technology upgrades will also need to be considered in the setting of more advanced informatics platforms. It is also recommended that all new technologies be tested in a simulation laboratory prior to purchase.4
Conclusion
The goal of intensive care is to provide the highest-quality treatment, in order to achieve the best outcome for critically ill patients. Research supporting the impact of the built environment has exerted a strong influence on multidisciplinary design teams as they seek solutions to maximise operational efficiency and create supportive healing environments for patients, families and clinical staff. The ICU is an ever-changing and rapidly advancing environment, with the integration of advanced informatics adding a new layer of complexity to design planning and operations. Future ICU designs will require planning for long-term flexibility by incorporating design decisions that accommodate changing care practices and information technology.
Authors
Diana C Anderson MD, MArch is an architect and medical planner at Stantec Architecture. Neil A Halpern MD, MCCM, FACP, FCCP is chief of the Critical Care Medicine Service, Department of Anesthesiology and Critical Care Medicine, at the Memorial Sloan Kettering Cancer Center, New York, NY. He is also Professor of Clinical Medicine and Professor of Medicine in Clinical Anesthesiology at Weill Cornell Medical College, NY.
References
- Halpern, NA and Pastores, SM. Critical-care medicine beds, use, occupancy, and costs in the United States: a methodological review. Crit Care Med. 2015; 25;43(11):2452–2459.
- Halpern, NA. Innovative designs for the smart ICU. Part 1: from initial thoughts to occupancy. Chest. 2014; 145(2):399–403.
- Halpern, NA. Innovative designs for the smart ICU. Part 2: The ICU. Chest. 2014; 145(3):646–658.
- Halpern, NA. Innovative designs for the smart ICU. Part 3: Advanced ICU informatics. Chest. 2014; 145(4):903–912.
- Hamilton, DK and Shepley, MM. Design for Critical Care: An Evidence-Based Approach. Burlington, MA: Elsevier Ltd; 2010.
- Ferri, M, Zygun, DA, Harrison, A and Stelfox, HT. Evidence-based design in an intensive care unit: end-user perceptions. BMC Anesthesiol. 2015; 15:57.
- Redden, PH and Evans, J. It takes teamwork. . . the role of nurses in ICU design. Crit Care Nurs. Q 2014; 37(1):41–52.
- Braun, D and Barnhardt, K. Critical thinking: optimal outcomes through end-user involvement in the design of critical-care areas. Crit Care Nurs. Q 2014; 37(1):33–40.
- Ulrich, RS, Zimring, C, Barch, XZ, Dubose, J, Seo, HB, Choi, YS, Quan, X and Joseph, A. A review of the research literature on evidence-based healthcare design. HERD. 2008; 1(3):61–125.
- Guidelines for design and construction of hospitals and outpatient facilities. 2014 edition. The Facilities Guidelines Institute. Dallas, TX; 2014.
- Thompson, DR, Hamilton, DK, Cadenhead, CD, Swoboda, SM, Schwindel, SM, Anderson, DC, Schmitz, EV, St Andre, AC, Axon, DC, Harrell, JW, Harvey, MA, Howard, A, Kaufman, DC and Petersen, C. Guidelines for intensive care unit design. Crit Care Med. 2012; 40(5):1586–1600.
- Award-winning ICU designs. How to build a better facility for patients and caregivers. 2016. www.sccm.org
- Cadenhead, CD and Anderson, DC. Critical-care design: trends in award-winning designs. World Health Design. 2009. Available from: http://www.worldhealthdesign.com/critical-care-design-trends-in-award-winning-designs.aspx
- Rashid, M. Two decades (1993–2012) of adult intensive-care unit design: a comparative study of the physical design features of the best practice examples. Crit Care Nurs. Q 2014; 37(1):3–32.
- Evans, J and Reyers, E. Patient room considerations in the intensive-care unit: caregiver, patient, family. Crit Care Nurs. Q 2014; 37(1):83–92.
- Lavender, SA, Sommerich, CM, Patterson, ES, Sanders, EB, Evans, KD, Park, S, Umar, RZ and Li, J. Hospital patient room design: the issues facing 23 occupational groups who work in medical/surgical patient rooms. HERD. 2015; 8(4):98–114.
- Maze, C. Inboard, outboard, or nested? Healthcare Design Magazine. 2009 (1 March, 2009). Available from: http://www.healthcaredesignmagazine.com/print/article/inboard-outboard-or-nested
- Reiling, J, Hughes, RG and Murphy, MR. The impact of facility design on patient safety. In: Hughes, RG (ed). Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality (US). 2008.
- Pati, D, Evans, J, Waggener, L and Harvey, T. An exploratory examination of medical gas booms versus traditional headwalls in intensive-care unit design. Crit Care Nurs. Q 2008; 31(4):340–56.
- Drews, FA. Human factors in critical-care medical environments. In: Morrow, DG (ed). Reviews of Human Factors and Ergonomics. Santa Monica, CA: Human Factors and Ergonomics Society. 2013; 103–48.
- Callahan, CW, Repeta, RJ Jr and Sherman, SS. Evidence-based building design and organisational culture. Front Health Serv Manage. 2014; 31(1):47–54.
- Johansson, L, Bergbom, I and Lindahl, B. Meanings of being critically ill in a sound-intensive ICU patient room – a phenomenological hermeneutical study. Open Nurs J. 2012; 6:108–16.
- Leaf, DE, Homel, P and Factor, PH. Relationship between ICU design and mortality. Chest. 2010; 137(5):1022–7.
- Lu, Y, Ossmann, MM, Leaf, DE and Factor, PH. Patient visibility and ICU mortality: a conceptual replication. HERD. 2014; 7(2):92–103.
- Perme, C and Chandrashekar, R. Early mobility and walking program for patients in intensive-care units: creating a standard of care. Am J Crit Care. 2009; 18(3):212–21.
- Kamel Boulos, MN and Berry, G. Real-time locating systems (RTLS) in healthcare: a condensed primer. Int J Health Geogr. 2012; 11:25.
- Halpern, NA and Brentjens, T. Point-of-care testing informatics. The critical-care hospital interface. Crit Care Clin. 1999; 15(3):577–91.
- Sturdivant, L and Warren, NA. Perceived met and unmet needs of family members of patients in the pediatric intensive-care unit. Crit Care Nurs. Q 2009; 32(2):149–58.
Organisations involved


