Healthcare / Service redesign
Thailand Healthcare System by Design: An integrated approach
By Surapong Lertsithichai, Mingmada Nayanakawee, Fontip Watcharaporn and Sarunporn Tongsubanan | 04 Sep 2023 | 0
This paper describes research initiated to analyse current problems and demand of healthcare stakeholders in Thailand.
Authors of scientific paper:
Abstract
With an increase in the elderly population and changes in epidemiology, it’s anticipated that the Thai population will develop more chronic diseases, and, consequently, the health system will become less effective. Thailand has created a healthcare system with a balanced population in mind, deploying a primary care system designed to accommodate preliminary illnesses and alleviate crowded situations in large hospitals, leaving more room for effective care for the elderly. However, the reality is the Thai population still prefers their health services delivered at large hospitals and is less concerned about health prevention, which are contributing towards an imbalance in the health system.
The Healthcare System by Design research was initiated with the objective to analyse current problems experienced by healthcare stakeholders in Thailand. Using the Healthcare Center at Chulalongkorn University as a case study, the intention was to develop an improved healthcare system through an integrated design approach with primary stakeholders involved in the development process. A series of co-creation workshops was conducted with primary stakeholders to design the ideal healthcare system. The findings revealed challenges in all components of the healthcare system, including health service, health workforce, medical products, vaccines and technologies, and health information.
Based on this analysis, a conceptual framework for a desired primary healthcare system was developed and a prototype system proposed. The framework is modelled using a master flow chart, a relationship diagram, and multiple wireframe diagrams to illustrate how the system is experienced from a user’s point of view. The data-driven integrated design prototype covers all primary care services, including treatment, health promotion and restoration, illness prevention, and combines knowledge from all stakeholders.
Keywords
It should be a human right that every person is entitled to a basic level of healthcare in each country, and therefore each state is required to provide quality healthcare services for its citizens. The healthcare system plays a crucial role in maintaining, promoting, and restoring the health of the population through various activities. There are six important components of the healthcare system, which include service delivery; the health workforce; information; medical products, vaccines and technology; financial; and leadership/governance.1
Each country has a different healthcare system depending on its appropriateness. Although many countries have made efforts to create healthcare systems that are accessible to the public, there is still inequality in accessing services.2 Thailand, on the other hand, has a diverse healthcare system, which makes healthcare services widely available and accessible to its population. According to the World Health Organization, Thailand has a high level of healthcare coverage compared with other countries in Asia.3 Also, according to data from the National Statistical Office in 2019, 99.3 per cent of the Thai population received universal health coverage, with the highest coverage provided by the universal health card or gold card – a programme that has been implemented since 2002.4,7
Although healthcare access coverage in Thailand is high, the diversity of healthcare systems with different principles, ideas and designs has resulted in inequalities in access to healthcare services. This leads to higher rates of hospital visits, causing issues such as overcrowding in hospitals, long wait times for medical services, and shortages of healthcare personnel, particularly in tertiary hospitals. However, regarding the healthcare service structure, Thailand has designed a healthcare system that covers all levels of hospitals, including primary, secondary and tertiary levels, according to the complexity of health problems.5 These three systems are linked together through a patient referral system.
In this regard, the primary healthcare service system plays a crucial role as the first line of care for basic illness treatment and promotion of recovery, and prevention of illnesses, with the aim of reducing the workload and congestion of hospitals. The system is distributed to regional areas to provide comprehensive services, despite the structural division of service levels. However, congestion in district hospitals is still high, owing to public confidence in the potential and quality of healthcare services at the district level being higher than that of the primary level. Additionally, patient referral systems haven’t been sufficiently smooth, and the ease of access to information today has allowed the public to educate themselves and make decisions more easily, leading to higher expectations for services and resulting in increased complaints.6
The important challenges, which many regions of the world, including Thailand, are facing, involve changes in population structure and epidemiology. In other words, Thailand is entering an ageing society where the population tends to have more chronic diseases, despite having a primary healthcare system designed to support basic illness management to alleviate the burden on large hospitals and enable universal access to healthcare services. Furthermore, there is an important role in promoting and preventing health to avoid illness. In reality, however, Thai people prefer to use services in large hospitals, leading to an imbalanced health system structure. Researchers have therefore recognised the importance of a primary healthcare system, combined with the current role of data management technology, in effectively improving the complex health system.
The objective of the integrated health system design project is to analyse the problems and needs of stakeholders in the primary healthcare system. Chulalongkorn University Health Service Center is a case study, and the information gathered will be presented to stakeholders to collectively develop a healthcare system prototype through an integrated design process. Ultimately, the goal is to use data analysis from all sectors involved to efficiently improve the national healthcare system.
Methodology
The research methodology conducted is both qualitative and quantitative, and follows an extensive process, as seen in Figure 1.
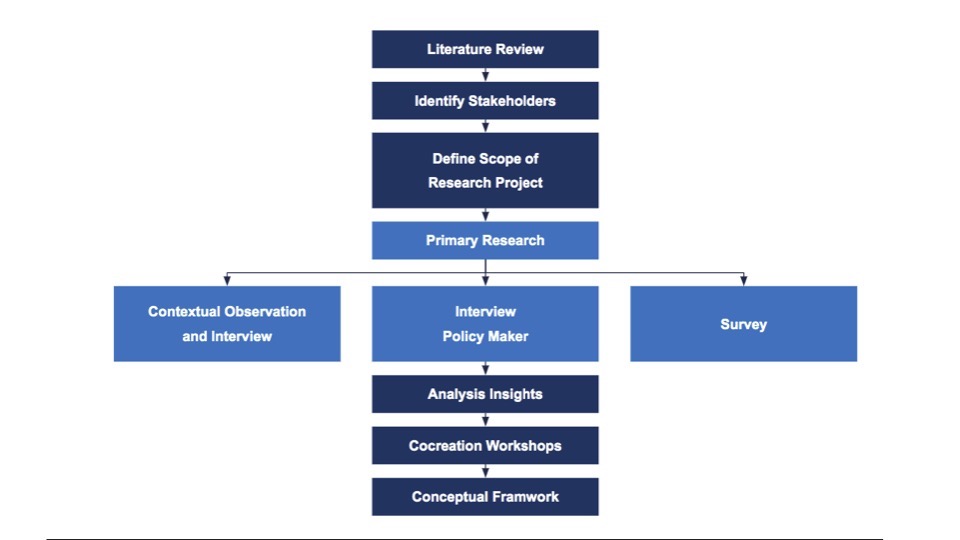
Qualitative and quantitative data collections were conducted, starting with a review of related literature, both in the context of Thailand and other countries. Operational meetings were then held with relevant parties within Chulalongkorn University to identify primary stakeholders. Qualitative data collection was carried out through observation and semi-structured interviews, with service providers and service recipients at the Chulalongkorn University Healthcare Center. Split into groups of ten, with ten policy-related healthcare workers, 30 people in total were interviewed on three topics: 1) opinions on changing the recording of data in digital format; 2) the format of healthcare services in the future; and 3) changes in service processes that would be most desirable.
Next, using the data obtained from observation and interviews, a process model of service providers and recipients was created. For quantitative data collection, a survey was conducted with three groups, including 329 randomly selected service recipients during business hours, 29 service providers, and 68 policy-related healthcare workers. The questionnaire covered general information, experiences related to health data recording, and opinions on personal health records.
Research stakeholders and participants
For the purpose of designing the healthcare system, the researchers identified primary stakeholders as:
- service recipients, including students, university staff, and the general public;
- service providers, including physicians, dentists, nurses, assistant nurses, medical assistants, pharmacists, physiotherapists, medical technicians, and healthcare support staff;
- related departments at Chulalongkorn University involved in providing healthcare services, including the Healthcare Center, the Center for Sports Science and Rehabilitation, the Faculty of Sports Science, the Dental Innovation Center, the Faculty of Dentistry, the Osotspa Clinic, the Faculty of Pharmacy, the Medical Technology Clinic, the Physical Therapy Clinic, and the Faculty of Medicine; and
- other personnel involved in health policy development, health information, and health technology.
Co-creation workshops
After collecting sufficient data and analysing patterns, a collaborative design workshop followed, designed to create a participatory design process involving stakeholders in the primary healthcare system, as seen in Figure 2.
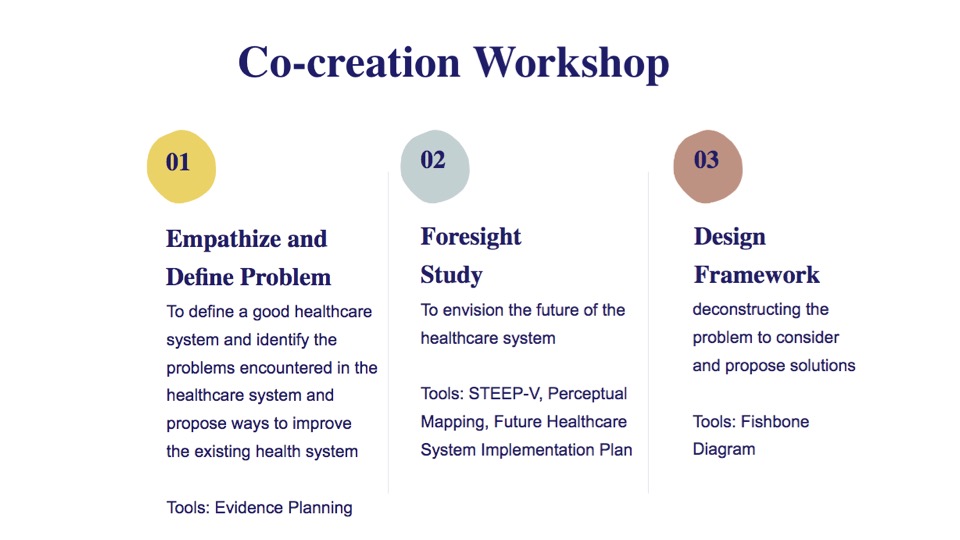
The workshop is divided into three sessions with the following objectives:
- to define a good healthcare system and identify the problems encountered in the healthcare system;
- to envision the future of the healthcare system; and
- to establish a framework for designing the healthcare system.
Co-creation workshop 1: Defining a good healthcare system
The first co-creation workshop sought to define a good health system and identify problems within the current health service system. Divided into two parts, the first part aimed to define a good health system, while the second part proposed ways to improve the existing health system. The first part examined the components of the healthcare system, which consisted of four main components out of six; namely, service delivery, health workforce, health information, and medical products, vaccines, and technologies. The second part sought to define problems using the evidence planning tool and analysing what constitutes a good healthcare system to improve the existing healthcare system.
Co-creation workshop 2: Foresight study of a healthcare system
The co-creation workshop to envision the future of the healthcare system was divided into three parts. The purpose was to identify changing trends in the healthcare system through the use of the ‘STEEP-V’ tool (Social, Technological, Economic, Environmental, Political, and Values), followed by a healthcare system foresight using the ‘Perceptual Mapping’ tool, and gathering opinions to create a ‘Future Healthcare System Implementation Plan’. The results from both workshops will be used to set the framework for designing the subsequent healthcare system.
Co-creation workshop 3: Healthcare System Design Framework
The last co-creation workshop was divided into three parts. The first part involved deconstructing the problem to consider and propose solutions by analysing it using the ‘fishbone diagram’, a chart that shows the relationship between the problem and all of its causes. The second part focused on designing solutions to the identified problems using problem-solving design techniques.
Research findings
Out of the interviews with the three groups, a consensus was reached that there should be a transition to digital health record systems that are accessible to all users, not duplicative, and which are easy to use. This must consider the elderly and other groups who may not have access to technology, as well as the linking of data between other organisations for convenience in data extraction, while data security is also essential.
The second issue, discussed among all three groups, is the format of the healthcare service system. This focuses on providing services through online systems that are convenient, fast and accurate, such as online appointments or online medical consultations, in order to reduce congestion of unnecessary hospital visits and the cost of travel for service users, as well as to support and promote public health so that people can receive basic first-aid training or take care of their own health. In addition, service providers want to have modern medical tools for treatment.
The third issue is the process of receiving services that needs to be improved. It was found that there is a desire to reduce the time and steps involved regarding documentation by using online systems; an example would be using only one ID card to access all relevant information, including online appointments and booking, to make the process easier for users.
Co-creation workshop results
The first co-creation workshop, to define a “good healthcare system” by analysing its components from the perspective of service users, identified four main topics. These can be summarised as follows: 1) Service delivery, which aims to provide comprehensive and efficient health services; 2) Health workforce, which aims to ensure workers have standardised and up-to-date knowledge; 3) Information, which aims to establish widespread and secure data linkage; and 4) Medical products, vaccines and technologies, which aim to meet the basic needs of future technology and coverage. The results of the feedback to improve the existing healthcare system suggest there is a need to boost the confidence of patients in the organisation, including building a good image of the service provider with standards that cover equal access to services. It was found that every issue has a common limitation: the budget to invest in or develop various potentials.
The second co-creation workshop showed that changing trends include those in the economy, environment, politics and values. It was found that in the social aspect, Thailand has entered the era of an aging society and is facing the situation of a Covid-19 pandemic outbreak, which has led to healthcare for patients at home and may result in proactive healthcare policies. Regarding technology, the Personal Data Protection Act (PDPA) law has recently been enacted, so now all personal data must be protected. Regarding the economy, since medical expenses are likely to increase, having comprehensive insurance coverage can help. Additionally, tourism and health-related products can support the economy. On the environment, the density of urban communities leads to the need for urban planning to find ways to eliminate infectious waste from the healthcare system. On politics, there must be participation from all sectors of the population, and regarding values, there must be equal service provision at all levels and for all social classes.
After considering “the future healthcare system”, it was found that the plausible future position is characterised by the horizontal line, which has a trend in providing health services that are location-based. The preferable future position, however, which is the expected future position, is characterised by the vertical line, which has a trend in providing health services that are not location-based and an increase in the production of personalised health products through information technology, as seen in Figure 3.
Having identified both positions, there is a gap between them that is further from the goal. Since it’s not possible to bring about changes in the short term, reaching the expected future goal will require a long period of time for these changes to occur. Thus, it’s necessary to consider and plan for short-term changes to enable continuous development and improvement of the healthcare system.
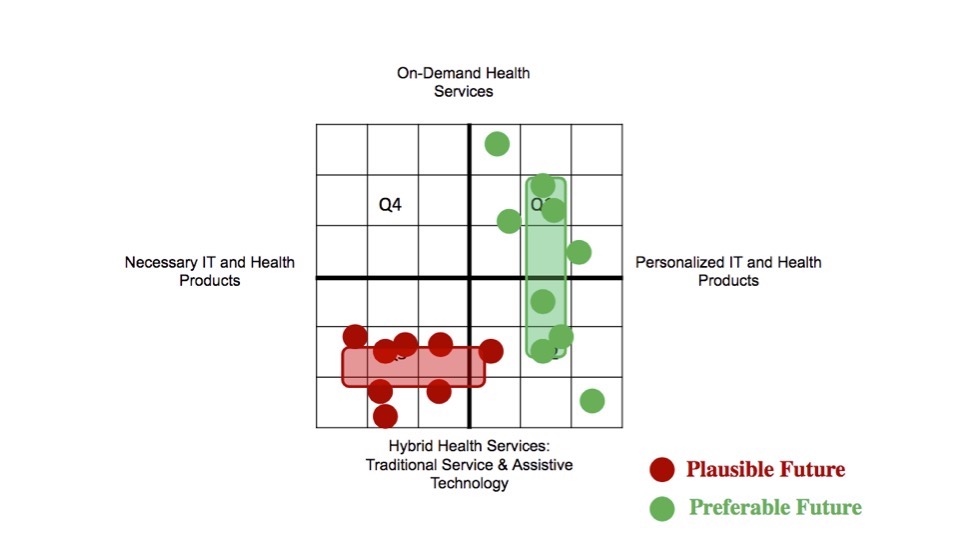
Results of the ‘Targets and approaches to achieving targets’ for the future health system service plan are divided into three phases, according to the framework of future outlooks. They show that a longer period of time will be needed to reach the goals set. Therefore, it’s necessary to take action in the short term by designing the framework of the health service system to create changes that will lead to the goals set for the future. The scope of the design work must be adjusted appropriately to fit the operational plan, and to accommodate suggestions for developing the health service system in various stages, in conjunction with overall system development.
The third co-creation workshop, defining a healthcare system design framework, began with ‘Part 1: Deconstructing the problem’, as seen in Figure 4. The result of identifying the problems of the components of the health system in all four areas found that: 1) service delivery – the problems found were services tied to location, inefficient queue management or scheduling, and limited access to health promotion services; 2) the health workforce – the problems found were workload overload and a lack of specialised expertise among personnel; 3) health information – the problems found were the inability to forward data between organisations, data redundancy, lack of patient identification evidence, and data insecurity; and 4) medical products, vaccines and technologies – the problems here were varied health equipment standards, policies limiting data access, access-level setting for practitioners, methods of measuring values using different equipment, and the misuse of medication or equipment. From the aforementioned, it leads to finding solutions to the problems of the health system’s components in all four topics in Part 2.
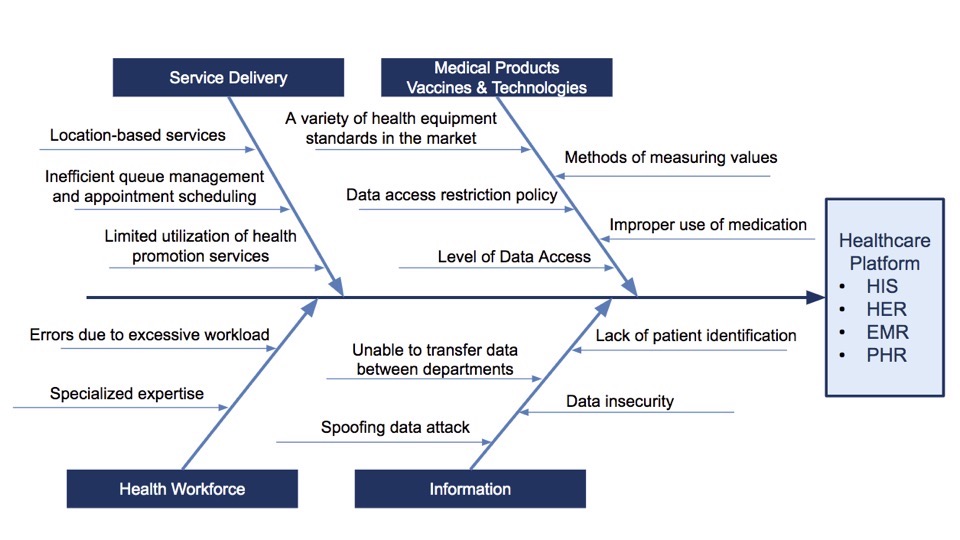
For ‘Part 2: Problem-solving design’, problem-solving guidelines were divided into four topics based on the components of the healthcare system, as follows:
Topic 1: Healthcare services – problem-solving guidelines for addressing issues in service provision through the use of telemedicine (tele-consultation) technology that enables patients and medical personnel to communicate in real-time, similar to teleconference communication. Both parties can see and talk to each other without limitations of time and location; easy, convenient, and saving time, patients still receive the same level of service as in hospital visits. Also included are the promotion, prevention and recovery policies to achieve comprehensive, complete and efficient healthcare services.
Topic 2: Health personnel – excessive workload may lead to errors resulting from limitations in specialised expertise. The solution is to alleviate the burden through technology and online systems, such as medication orders, appointment scheduling, reminders, and personal health records that store patient health data in electronic format, which patients can access and control, manage, and exchange information with others. Personalised care will make healthcare for each individual more effective to achieve standardised goals and up-to-date knowledge coverage.
Topic 3: Medical products – to achieve comprehensive, situation-appropriate, and secure data linkage, policies must be put in place to reduce inequalities in access to quality health devices. These policies will serve as a bridge to using technology as a medium to help patients and medical personnel communicate in real-time (telemedicine) and manage personal health records electronically. This is the use of information technology to support the effectiveness and management of health service systems, and to facilitate the exchange of health information through immediate, accurate and legally compliant standards under the PDPA. In addition, this also includes promoting knowledge, providing health advice, and ensuring proper use of medication and equipment.
Topic 4: Information technology data, guidelines for addressing coverage, and adequacy based on technological support in the future must be under the PDPA law to secure personal health records, electronic data and personalised care that requires data management technology assistance, with clear and secure access and identity verification systems.
It was found that the main solution to these problems is to use technology to help patients and medical personnel solve and manage them. These solutions include telemedicine, personal health records, electronic data, and personalised care under the PDPA law. Additionally, this also includes promoting basic knowledge policy and reducing inequality in accessing healthcare services. These solutions can help improve the efficiency of the healthcare system in the future, as expected.
In Part 3, the results of the consideration and proposal of the Health System Design Framework can be summarised, as shown in Figure 5.
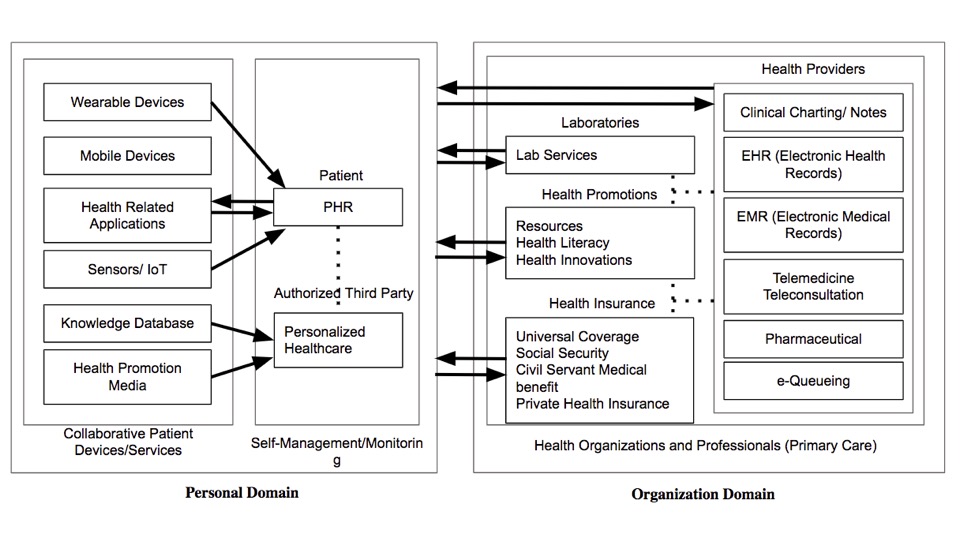
From the diagram, the health information system links the health information data from users and health organisations, including hospitals. The health information data from users is obtained from various health measurement devices, such as wearable devices, health applications, and body signal detectors. These data are stored in the personal health record dataset, as well as in the health information media database or datasets related to healthcare knowledge that have been customised to suit the user’s behaviour and lifestyle. Users can use this health information data to manage their health effectively.
The health information data from health organisations includes datasets from laboratories and databases sent to promote health. The dataset from both public and private health insurance is included, and the dataset from hospitals – such as medical diagnoses, medical histories, electronic health records, and medical care, including telemedicine, medication information, queue management, and various datasets – are linked and exchanged with each other, which can be used to monitor and provide healthcare services.
Discussion
To summarise the research findings, both the possibilities and obstacles of using data-driven health systems depend on overcoming micro and macro challenges within the existing healthcare system. By collecting data and conducting interviews with healthcare personnel, it has been shown that there are problems and obstacles preventing the linkage of data between hospitals and departments, owing to the use of different operating systems. This creates redundant work processes, so a solution would be a central standardised system that can link with various information systems seamlessly. Additionally, both service providers and recipients consider data security to be a crucial issue because health data is sensitive and requires strict protection. Therefore, a centralised agency should be responsible for managing and protecting the health data of recipients, with clear levels of access rights for different stakeholders. For instance, caregivers have access to the data of those they are taking care of; doctors can access treatment history, laboratory test results, and medication history; etc. Blockchain technology is one solution to ensure data security and management, including financial transactions. However, there are still challenges regarding accessibility and usability of technology, despite its rapid development.
Future research
In regard to expanding the reach of health services to other primary care settings beyond the university context, although organisational operational structures may differ in detail, there is a common approach to promoting public health. This includes health promotion, disease prevention, health maintenance, and health restoration. Expansion may begin with regular health data collection, emphasising preventive measures, and efficient health data collection tools are also crucial. The Government can play a crucial role in supporting and pushing for these changes. To continue to achieve desirable outcomes from this framework, additional research is necessary, such as designing effective health outcome measures and studying cost-effectiveness. The results of such research will benefit stakeholders, including policymakers in the education and healthcare fields, and address arising issues to plan future development frameworks with greater detail.
In integrating a data-driven approach to the design of a healthcare system, using cutting-edge technology tools empowers individuals to take better care of themselves, prevent illnesses, and monitor their health regularly. This is achieved by designing a system that motivates individuals to record their health data, including complex and constantly changing big data, and using data analytics technology, such as machine learning and artificial intelligence, to analyse the trend patterns to identify potential health risks. For individuals with chronic conditions, such as diabetes, hypertension, and high cholesterol, healthcare providers can provide online advice and monitor their health through the use of online systems. This helps to build confidence in using healthcare services remotely and promotes health maintenance through regular monitoring and advice. It also empowers individuals to control and manage their health with the support of family doctors and healthcare providers.
Health data support continuous system improvements. By having exclusive access to their health data, individuals can control and take care of their health with personalised recommendations. By adopting this data-driven approach nationwide, healthcare providers can enhance the effectiveness of primary healthcare services, and ultimately improve population health outcomes, which lead to better health outcomes.
About the authors
Assist. Prof. Surapong Lertsithichai is a lecturer in design and architecture at the Faculty of Architecture, Chulalongkorn University in Thailand. Mingmada Nayanakawee is a senior researcher for the Faculty of Architecture, Chulalongkorn University. Dr Fontip Watcharaporn is physician and researcher at Thailand’s Institute for Urban Disease Control and Prevention. And Sarunporn Tongsubanan is a graduate student and PhD candidate at the School of Architecture, Art and Design at King Mongkut’s Institute of Technology Ladkrabang in Thailand.
References
- World Health Organization. (2007). Everybody’s business – strengthening health systems to improve health outcomes: WHO’s framework for action.
- Hfocus. (2013). Rabobb Sukhaphaph ASEAN: Rowm Kan Reng Phatthana Lak Prakan Sukhaphaph [ASEAN Health System: Accelerating the development of health security]. Retrieved from https://www.hfocus.org/content/2019/12/18250
- National Health Security Office. (2019). NHSO Annual Report, Fiscal Year 2019.
- National Statistical Office Thailand. (2019). The 2019 Health and Welfare Survey.
- Ministry of Public Health of Thailand. (2019). Rabobb Brikan Thanh Kan Phaet [Medical service system]. Retrieved from https://bkpho.moph.go.th
- Policy and Strategy Office, Ministry of Public Health. (2016). Thailand health profile, 2011–2015. Retrieved from https://hp.anamai.moph.go.th/
- Department of Health Service Support. (2019). National Health Insurance System Development Report. Retrieved from https://www.nhso.go.th/operating_results

