Healthcare / Healthy Cities
Reimagining the hospital: Building wellness – the whole more than the sum of its parts
By Prachi Rampuria, Danny Gibson, Kieren Morgan and Soham De | 20 May 2022 | 0
Prachi Rampuria, Soham De, Danny Gibson and Kieren Morgan describe a set of creative principles that can help planners, architects, and engineers view hospital design through the lens of broader concepts, including wellness, population health, and urban design.
Authors of scientific paper:
Abstract
New potentials for building wellness are opening up, through initiatives to integrate health and care, currently driving a wholesale reorganisation of the NHS into geographically based integrated care systems incorporating primary, community, and secondary care facilities. International research on integrated care systems (ICSs) suggests that the future hospital should not be focused on one geographical location but should be dispersed to offer the population more accessible, tailored, and focused care and support. Healthcare facilities of multiple scales will be closely integrated with settlements throughout the region.
Purpose
The research aim is to develop planning and design principles, across a range of spatial scales (regional, neighbourhood, buildings) to enable these diverse healthcare facilities to integrate with their wider environments, so as to treat illness in ways that also support the building of underlying wellness.
Methods
The research employed an ‘Inquiry by design’ approach (Zeisel, J. 2006), with the involvement of medical and/or healthcare planners and designers, urban designers, and architects.
Results
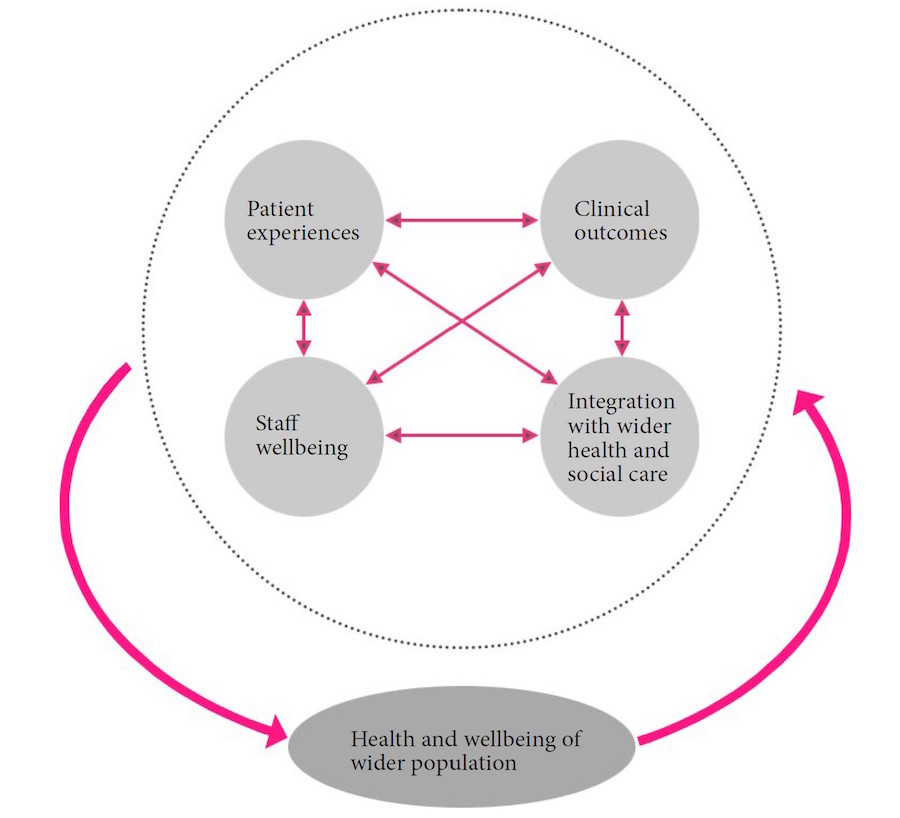
The research has developed design principles both at regional and neighbourhood scales that build on the NHS drive towards geographically based ICSs and enable healthcare facilities to form the seeds of neighbourhoods that foster wellness by supporting active lifestyles. Creating links between healthcare and the neighbourhood’s wider activities, these principles also have implications for the value of the NHS real estate. Potentially increasing the funding available for the hospital facilities themselves, this aspect will need much debate as these ideas are developed further. Finally, at the building scale, we develop design principles for the spatial structure and physical construction of the hospital elements themselves. Here we focus on improving patient experiences, clinical outcomes, staff wellbeing, and integration with wider health and social care at the most personal level.
Conclusions
The principles we have developed do not define a rigid recipe. Focused on creating positive relationships between the potentials of particular neighbourhood contexts and healthcare demands, their outcomes will depend on the nature of these potentials in each particular location. Used creatively, therefore, the same underlying principles will always generate situation-specific outcomes. There is, however, a common factor: these principles help the designer break free from the conception of the healthcare facility as an isolated element. The whole, in healthcare terms, becomes more than the sum of its parts.
Keywords
The NHS is facing unprecedented challenges. The Covid-19 pandemic has generated greater demand for healthcare than any period since the service was founded. A waiting list of 5 million now has to be addressed by increasingly exhausted front-line workers, against the backdrop of more than ten years of budgetary attrition and a large-scale reorganisation of the 2012 Health and Social Care Act, which many feel was an unnecessary and damaging failure.
To make matters worse, these challenges must be addressed in the context of widening threats to public health. Current ways of life are damaging natural capital’s capacity to regulate climate, and are disrupting natural systems in ways that threaten us with future pandemics. In the employment sphere, artificial intelligence is rapidly reducing demand for all but highly skilled workers – generating a precariat trapped in poverty and low job satisfaction, impacting on the mental health of both individuals and wider communities, and leaving many people trapped between endemic loneliness and a pervasive sense of stranger-danger. Housing, too, is problematic: one in three people in the UK live in poor-quality homes with negative health impacts, which are estimated to cost the NHS £1.4bn a year1.
Compounding this situation, many NHS providers are doing their best to deliver an ever-greater complexity and volume of care from a healthcare estate, which, in large parts, is well past its best. Long-term lack of capital investment means that providers are using out-of-date buildings, no longer fit for purpose and with a huge maintenance backlog2. They struggle to deal with the demand for care while responding to developments in clinical best practice and in new technologies that are needed to improve care quality. In many instances, they cannot provide patients with the basic elements of a satisfactory healing environment.
The NHS estate faces a confluence of interrelated pressures: a need for extensive investment; a political commitment to provide significant but still limited resources; yet another major organisational restructuring that will significantly affect the way that care is provided and capital investment managed; and the immediate need to continue to respond to the worst pandemic in a century and to recover from its wider impacts on healthcare provision. Clearly, this is a time that demands new thinking about hospital planning and design.
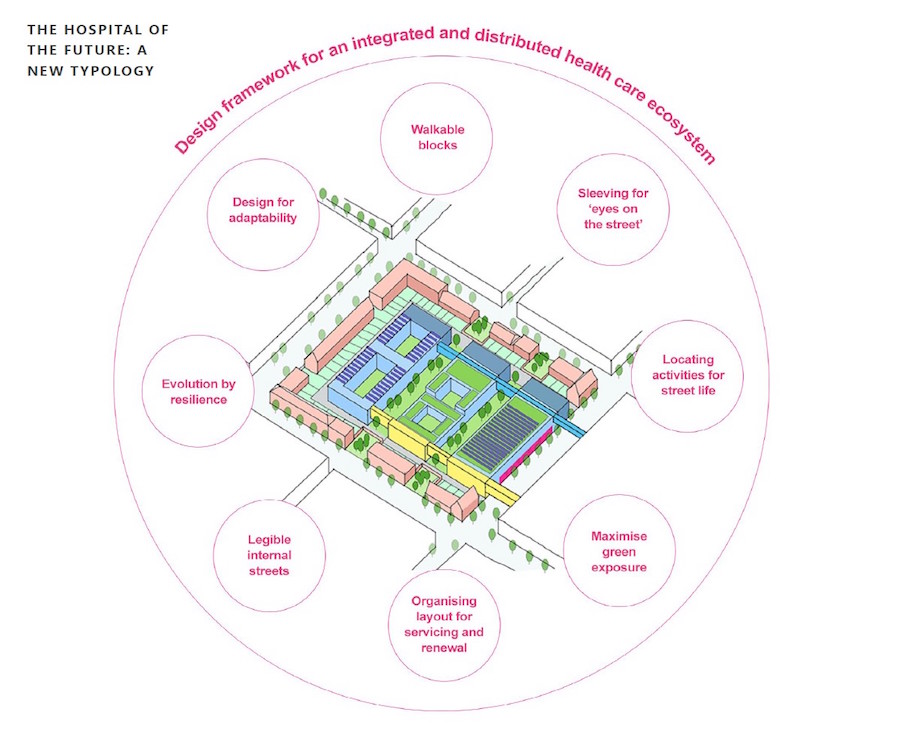
Design aims
This situation calls for fresh principles for designing and planning new hospitals to support radically improved patient experiences, clinical outcomes, staff wellbeing, and integration with wider health and social care, in environmentally sustainable and economically feasible ways. All these aspects of hospital performance are tightly interlinked: design decisions that affect any of them will probably affect them all. They also relate primarily to the hospital’s effectiveness in treating illness. Ultimately, however, the outcomes of treatment must depend on the patient population’s underlying levels of health and wellbeing. For maximum cost effectiveness, therefore, we need new design ideas that increase hospitals’ capacity to treat illness in ways that also help to build wider wellness (see Fig.1).
To develop these new ideas, we need to define both ‘hospital’ and ‘design’ in ways that free our thinking from current preconceptions as much as possible. We therefore define ‘hospitals’ as ‘settings for healthcare’ at any scale, and we understand ‘planning and design’ as ‘attempting to transform a current situation into a desired new one’3.
 A broader economic frame
A broader economic frame
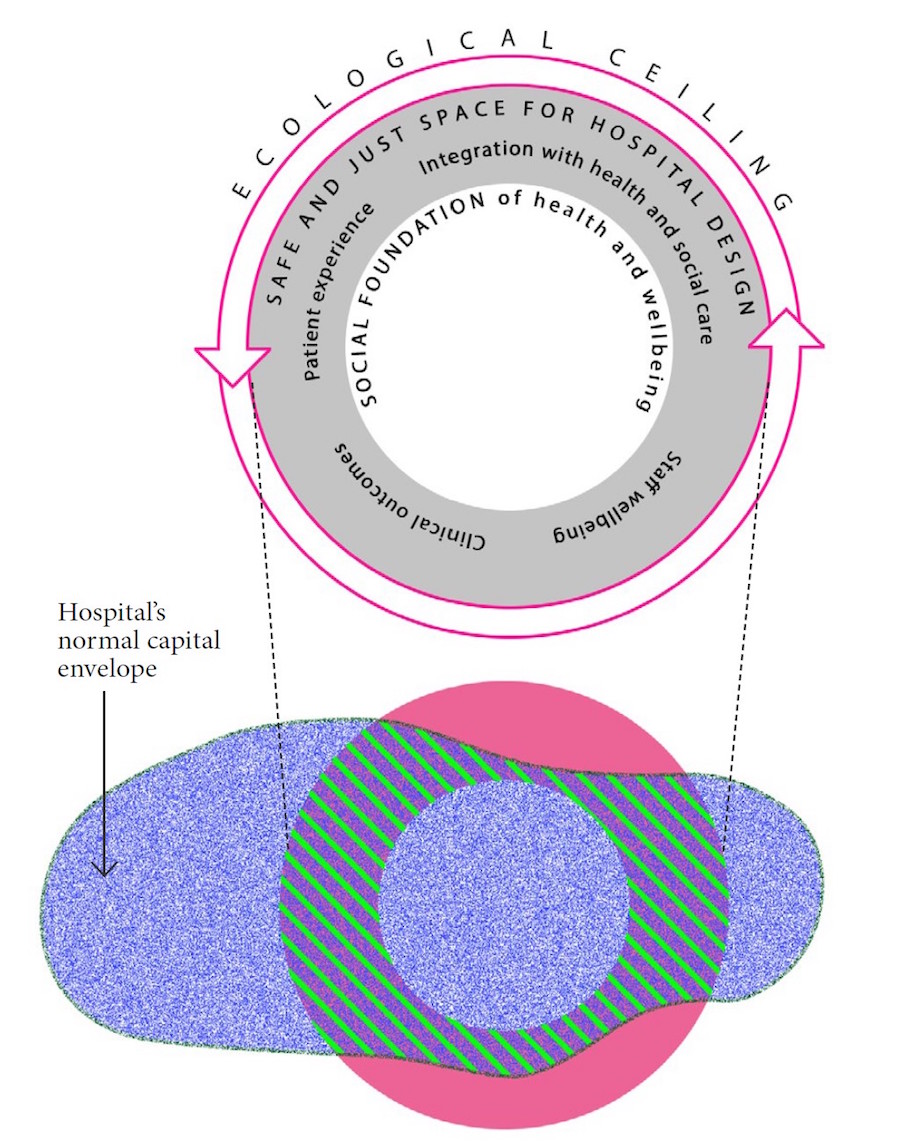
We also need a broad economic frame to guide our thinking about resource-allocation in relation to the opportunities and threats that health and wellbeing currently face. The most useful framework, developed by Kate Raworth, highlights the “safe and just space” between a “social foundation” of health and wellbeing, and an “ecological ceiling” on which human survival ultimately depends4. Within this space, Raworth focuses our attention on the need for distributing resources in circular, regenerative ways. Within this overall frame, continuing financial restrictions require design ideas that must also fit inside the normal capital envelope within which hospitals are developed (see Fig.2 and Fig.3).
Meeting the challenges
Research5 indicates that health systems throughout the world have historically been designed primarily to deal with single, acute and short-term illnesses, leading over time to fragmented healthcare operated by multiple organisations. Such a model cannot meet the demands of modern populations, especially the elderly, many of whom have higher levels of dependency, multiple long-term conditions, dementia, and complex co-morbidity. It has become apparent that these systems are becoming increasingly ineffective and inefficient, with escalating costs and poor patient experiences.
In the UK, as in many other countries, there is growing agreement that the way forward is to integrate systems of health and social care so that the whole becomes more than the sum of its parts. To date, the NHS has seen integrated care models implemented only as time-limited, geographically specific or care-pathway specific pilot projects, often with limited impact on the wider delivery of services. There is now, however, a renewed impetus at national government level to push ahead with the integration of health and social care through a wholesale reorganisation of the NHS into geographically based integrated care systems, incorporating primary, community and secondary care facilities.
In November 2020, in line with the 2019 NHS Long Term Plan, the NHS leadership set a firm deadline for the rollout of this programme, targeting the statutory establishment of integrated care systems in England by April 2022. This approach will see commissioners and providers of healthcare services for a defined regional geographical area collectively planning and integrating care provision to better meet the needs of their population. Opportunities for deeper integration of services to provide preventive, anticipatory and responsive support and care are being explored and developed at unprecedented pace.
International exemplars
In the context of this ambitious path towards a reorganised NHS, it’s important to learn lessons from other parts of the world where the provision of integrated services is further advanced. Research6 has found that in many instances, as in the NHS, the function, use and location of the estate is still largely considered in silos, despite a systemic transformation to an organisational shift towards integrated care. Organisational change, it seems, is necessary but not sufficient for the development of new, more integrated models of health and care delivery. Spatial thinking is also needed. 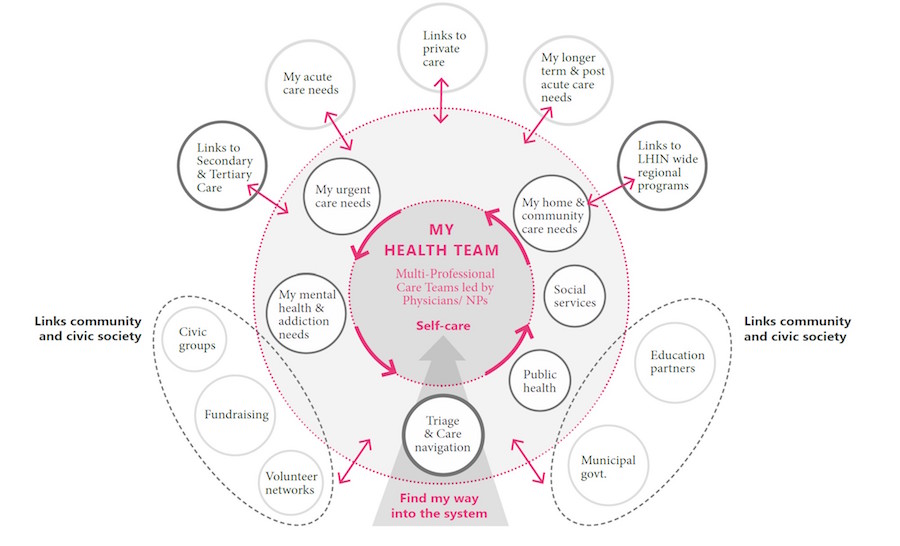
Some countries, however, are also developing new spatial models that seek to integrate care, improve patient satisfaction, and make effective and efficient use of resources with a renewed focus on wellness and prevention. These models typically incorporate: primary care networks; mental health; housing and social benefit support centres; integrated living accommodation for all generations; supported living housing; as well as facilities for secondary and acute care. Two positive examples can be seen in the very different contexts of Muskoka, Canada and Luohu, a district of Shenzhen, China.
Muskoka, Canada
In Muskoka, the model of care7 is a broad-based community effort, centred on ‘My Health Team’, a primary care-led, multi-professional team, focusing on wellness care and self-management (see Fig.4). The individual, their family and caregivers are at the centre of the service model, supported by the My Health Team. A new single integrated governance model has been created and is described as the ‘collective impact’ approach – through which a diverse group of individuals from the health, social, community, and local authority sectors come together to deliver: better health for the entire population; better care for individual patients; better value for the entire care system; and better experience for the individual care providers. Horizontal and vertical service alignment, along with strong communication, ensures seamless integration between physical health and mental health; easier navigation of the system; and no repeated assessment and co-ordinated access to primary, urgent and acute care services. Digital health and technology-based processes and wearable devices and tools support this model and help streamline the process to bring services closer to home, especially in rural and remote communities. 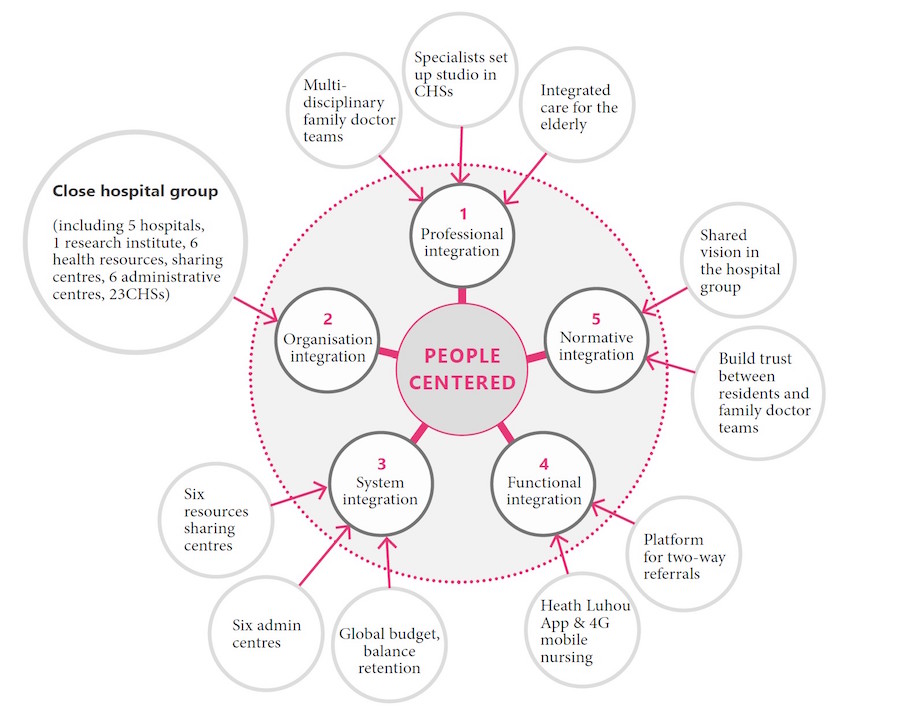
Luohu, China
Luohu is one of the ten districts in China’s Shenzhen region, with an area of 78.36km2 and a population of 1.4 million. With a fragmented health system, the key strategy was the establishment of an independent healthcare management group to oversee all healthcare in the district8. The group developed a health system of five hospitals, one institute of medicine and 23 community health centres restructured into a single Luohu Hospital Group, which is responsible for its funding and management (see Fig.5). The Group switched emphasis from curing disease to preventive healthcare, and by reorganising the 29 facilities, the restructure guaranteed at least one regional comprehensive medical centre and one primary medical group in each area of the district, as well as a healthcare centre in each community. The key features of the Luohu model include a hospital management centre, to perform the decision-making functions on behalf of the municipal government, across the entire spectrum of health rather than only across the hospitals. This recalibrates resources from acute, secondary facilities to the community, reflecting a shift to provide healthcare and support closer to home.
This is translated into the workforce for system delivery at various levels. The hospital management centre, for example, supports the principle of integrated personnel management, on the basis of which the doctors, as employees of the Luohu Hospital Group, move freely among the community centres, after one year training of general practice and health management. Evaluation after the first two years showed improvement in organisational effectiveness through integrated care. Moreover, new preventive programmes resulted in the reduction of disease incidence, and residents were more satisfied with services provided by the new model.
Common factors
It’s evident from comparative research9 that successful models of integrated care such as Muskoka and Luohu typically incorporate: primary care networks; mental health; housing and social benefit support centres; integrated living accommodation for all generations; supported living housing; as well as facilities for secondary and acute care. Common to all the care models reviewed is the extensive and growing use of digital technology, artificial intelligence and big data: successful integrated health and care systems rely on digital information recording and sharing platforms.
The digital dimension
Accelerated by the pandemic, the NHS is already on a path to digital transformation10, recognising the need for an integrated and editable patient record to resolve information asymmetry and fragmentation between providers. The development of this essential foundation for building an integrated care system is therefore in hand.
The digital platform allows healthcare to be integrated spatially with the demographics of the region’s population: wearable devices, big data and AI will refocus on health at home and therapeutic support in healthcare settings as close as possible to the patient. This will be beneficial not only for the patient experience but also in improving clinical outcomes through the provision of a co-ordinated delivery of health and care. It will also impact positively on the climate emergency and on air pollution, by reducing the amount of travel necessitated by current models of care.
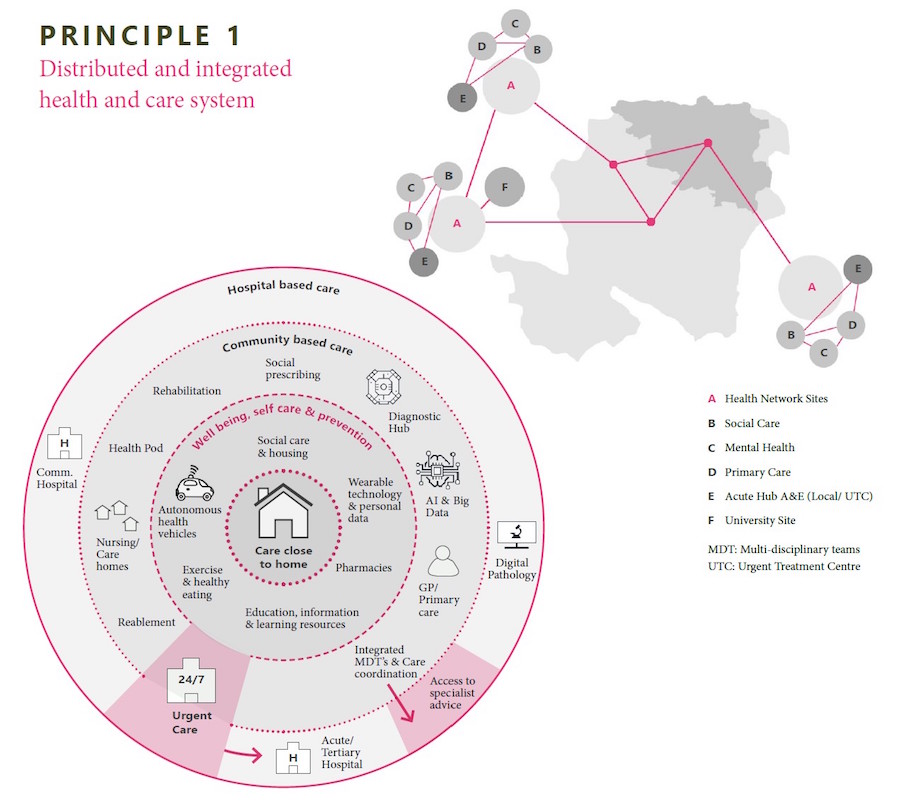
The care pathway is therefore kept in the community or at home as far as possible, while secondary care is provided when needed, supported by technology, such as telemedicine and wearable devices, and local multi-agency support is co-ordinated through a dedicated ‘health and wellness manager’. All this suggests that the future hospital will no longer be focused on a single geographical location but will be disaggregated to offer the population more accessible, tailored and focused care and support. This generates our first and largest-scale design principle: A distributed and integrated health and care system (see Fig.6).
Implementation
Research suggests11 that the optimal implementation of this first principle depends on the spatial demography of the region concerned. Where the population is dispersed through villages and small towns, services are best distributed through a geographically spread ‘hub and spokes’ approach. Where the population is concentrated in large centres, however, integration is best achieved by concentrating services in larger health campuses. Both approaches are relevant to the UK context with its mix of city or urban conurbations and more widely spread rural communities.
This first principle suggests an agenda for creative NHS thinking at the regional scale. In the short term, however, it seems likely that this scale of thinking will be overwhelmed by the speed of decision-making required by the Government’s current Health Infrastructure Plan (HIP), published in September 2019, outlining proposals to redevelop 40 hospitals – later increased to 48 – and to change the way capital investment is allocated and managed.
While the HIP programme was desperately needed, even prior to the pandemic, Covid-19 has increased both the extent and urgency of the changes required. Many NHS trusts are therefore racing forward with business cases for their capital development plans, in order to secure HIP allocations, with little time to digest new ideas that have large-scale implications. It’s therefore important to draw out smaller-scale design principles to start rethinking NHS real estate bottom-up, to create distributed integrated care systems incrementally, at the neighbourhood scale.
Moving to the neighbourhood scale
Even when they form well-distributed systems at the regional scale, most hospitals have negative impacts on wellness at the neighbourhood scale. Typically, even the best-distributed hospitals are only loosely integrated with other neighbourhood activities (see Fig. 8, 9, 10, 11), which nudges people away from the physical exercise of active travel; it just seems easier to take the car. To build wellness, however, we need neighbourhood design that counters the obesity epidemic by fostering more active lifestyles.
At a closer focus, large impermeable hospital footprints put off pedestrians and cyclists by forcing them to make detours: blocks larger than 200 sqm will reflect this car-dependent impact12. To avoid this, we must look for opportunities to break down the hospital block size to walkable dimensions.
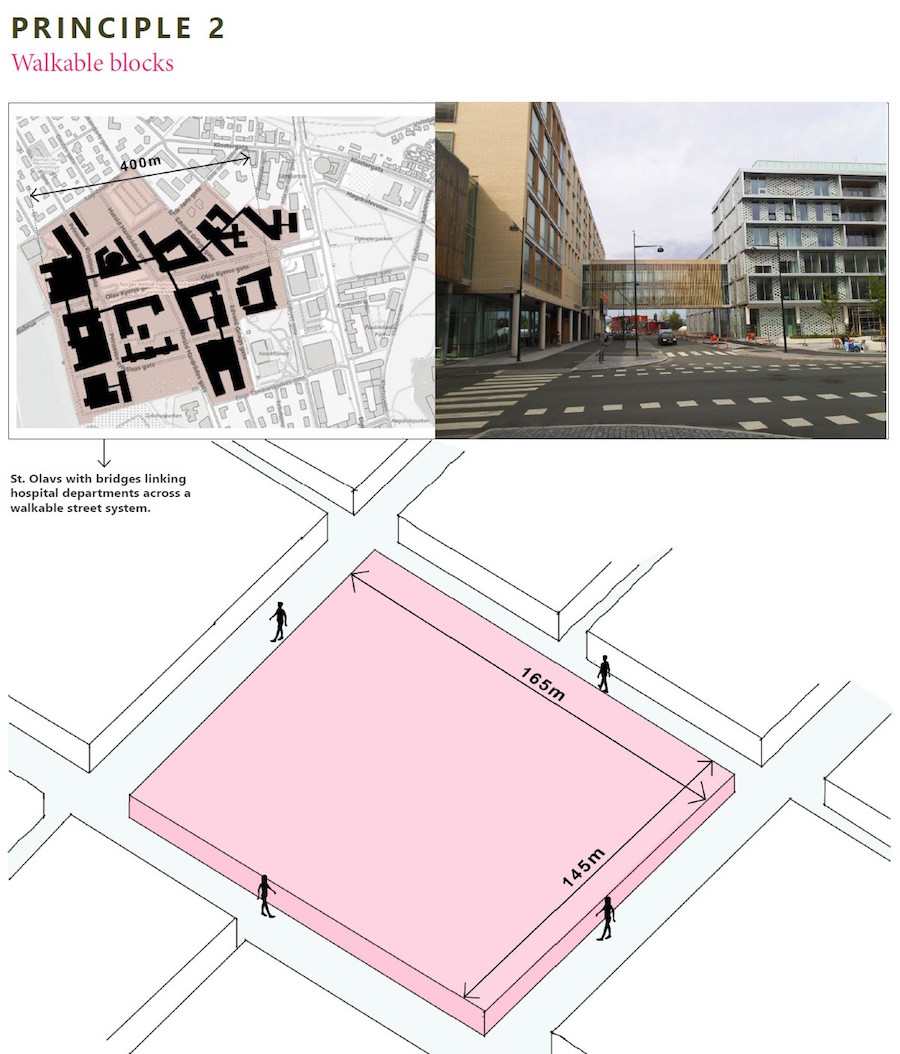
Several recent examples show how this can be achieved in the design of new hospitals, with bridges linking departments across a permeable street system. In the case of alterations to existing facilities, the starting point is to seek opportunities to create new streets through the site in the course of renewing outdated building stock. These considerations generate our second design principle: Walkable blocks (see Fig.7).
Walkability, however, requires more than just walkable-sized blocks. In these times of post-pandemic stranger-danger, we need reassurance to feel safe in using the streets without the protection of our cars. ‘Eyes on the street’ from people in adjoining buildings help keep us feeling safe13, but there is a problem here, too: most of the activities inside hospitals are too private to offer many eyes on the street. To maintain patient dignity, hospitals themselves are essentially introverted buildings. So, to provide eyes on the street, hospitals need to be ‘sleeved’ behind other activities such as housing, which can help convert the introverted hospital silo into an outward-facing wellness hub.
These more street-related activities offer the emerging hub a double advantage: unlike the introverted hospital edge, they create economic as well as social value from their street-edge location. There is a great deal of evidence to show that long thin strips of land alongside streets are highly efficient in property development terms14, so two birds can be killed with one stone here. As well as providing space for activities that benefit wellness-building – which might range from social housing to encourage recruitment of young doctors and nurses, through to special needs housing to reduce problems of bed-blocking, through to training spaces to help disadvantaged youngsters into work – there are opportunities for creative thinking about value capture to increase the financial viability of the emerging hub as a whole.
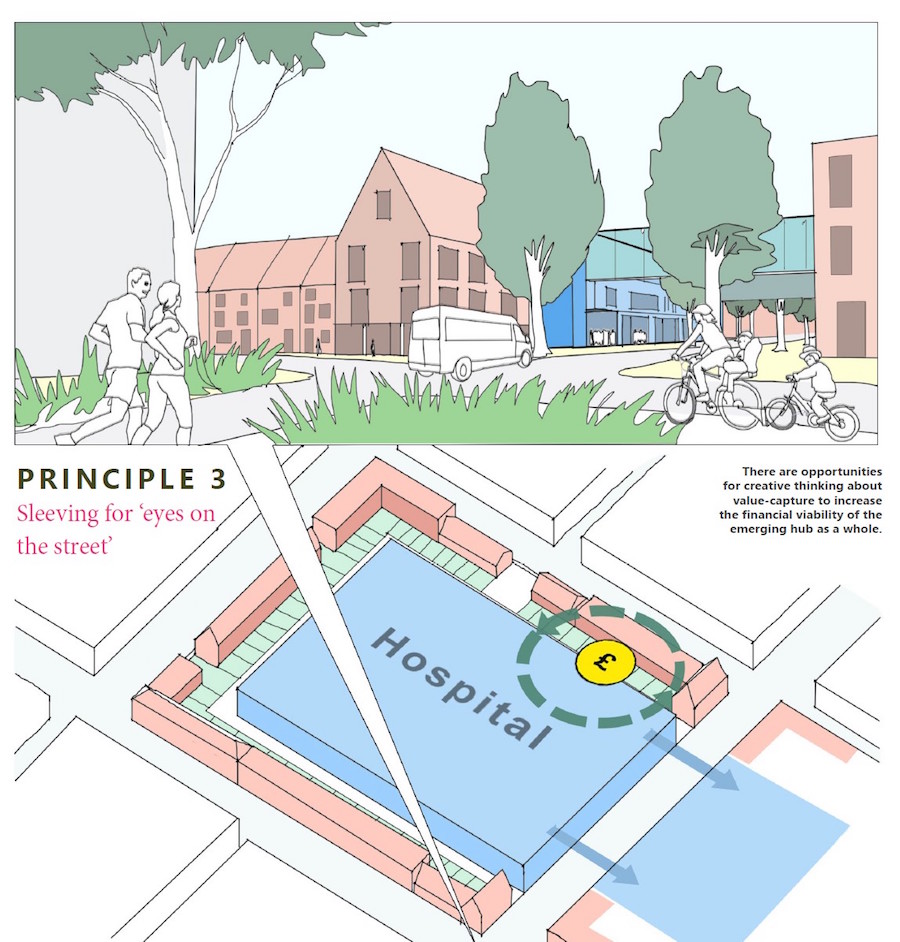
As these ideas are developed further, they will require intense debate to ensure that the economic tail does not start to wag the health and wellness dog. Taken together, these factors generate our third design principle: Sleeving for ‘eyes on the street’ (see Fig.8).
Protected by its sleeve, the hospital itself now occupies land within the block, with its own private road access distinct from the public street system, and with only one street edge of its own. For the liveliness of the street system as a whole, we must maintain eyes on the street along this edge15.
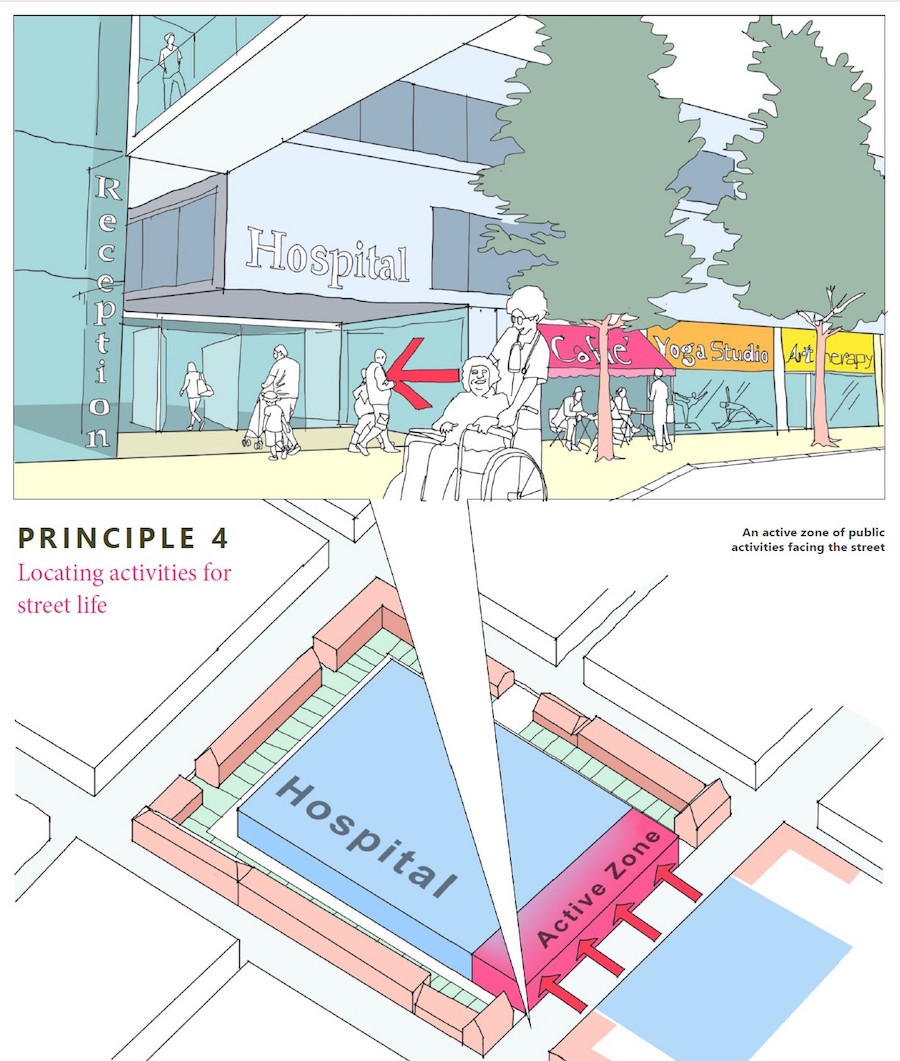
The ground floor, therefore, is where we locate public entrances, together with activities such as shops, cafe or gym, or studios for yoga or art therapy, which are valuable both for the hospital itself and for the wellness of the wider community. Activities such as spaces for hospital staff, which benefit from contact with everyday normality, can then take advantage of overlooking the street from upper levels. These considerations generate our fourth design principle: Locating activities for street life (see Fig.9).
Since the 1980s, it has been well known that hospital patients recover faster with views of nature than with views of brick walls, and we now know that green settings also reduce the levels of pain relief that need to be administered16. Green experience helps maintain and develop wellness, too; evolving in natural environments, it’s unsurprising that humans have developed a basic affinity with other natural systems, known as biophilia17. Because they help reduce stress18, green surroundings make for more harmonious, trusting relationships with others19, enabling us to develop cultural capital in the process. Wherever possible, therefore, our neighbourhood wellness hub should take advantage of opportunities for incorporating natural elements.
Since biodiversity benefits from connecting green elements to create green corridors20, the most cost-effective way of harnessing biophilia is by creating highly connected, tree-planted streets, reinforced, where possible, by exposed rainwater drainage swales. This has further wellness advantages in times of climate emergency – reducing urban heat island impacts through evapotranspiration and reducing the dangers of summer heat stroke, particularly for elderly people. Small-leaved trees and hedges can also significantly filter the current illegal level of particulate pollution from cars’ brakes and clutches – a level that seems set to continue into the age of the electric car and which is currently responsible for some 40,000 premature UK deaths each year21.
To maximise the connectivity of the system as a whole, to encourage the multisensory experience of birds, butterflies and pollinators, we can design these green corridors to pierce the hospital sleeve, flowing through into the internal spaces of the hospital itself. Where green corridors penetrate the sleeve, we can create small street-related pocket parks for well-surveilled children’s play and informal gatherings. Within the hospital itself, green corridors, about 20 metres wide, allow internal spaces such as wards to experience natural spaces while maintaining their own privacy22.
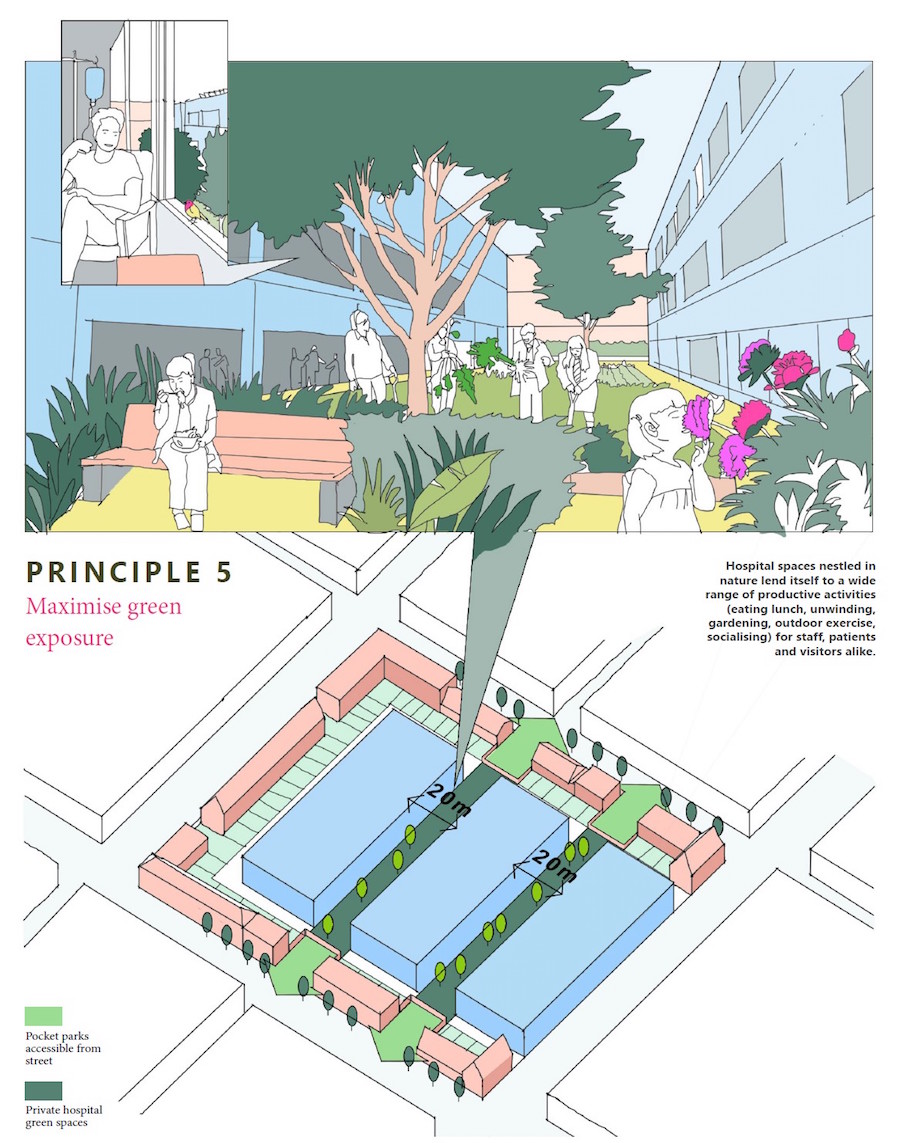
These green spaces also provide opportunities for local volunteers to engage in therapeutic gardening activities and, in the process, provide fresh produce for the hospital kitchen. These considerations generate our fifth design principle: Maximise green exposure (see Fig.10).
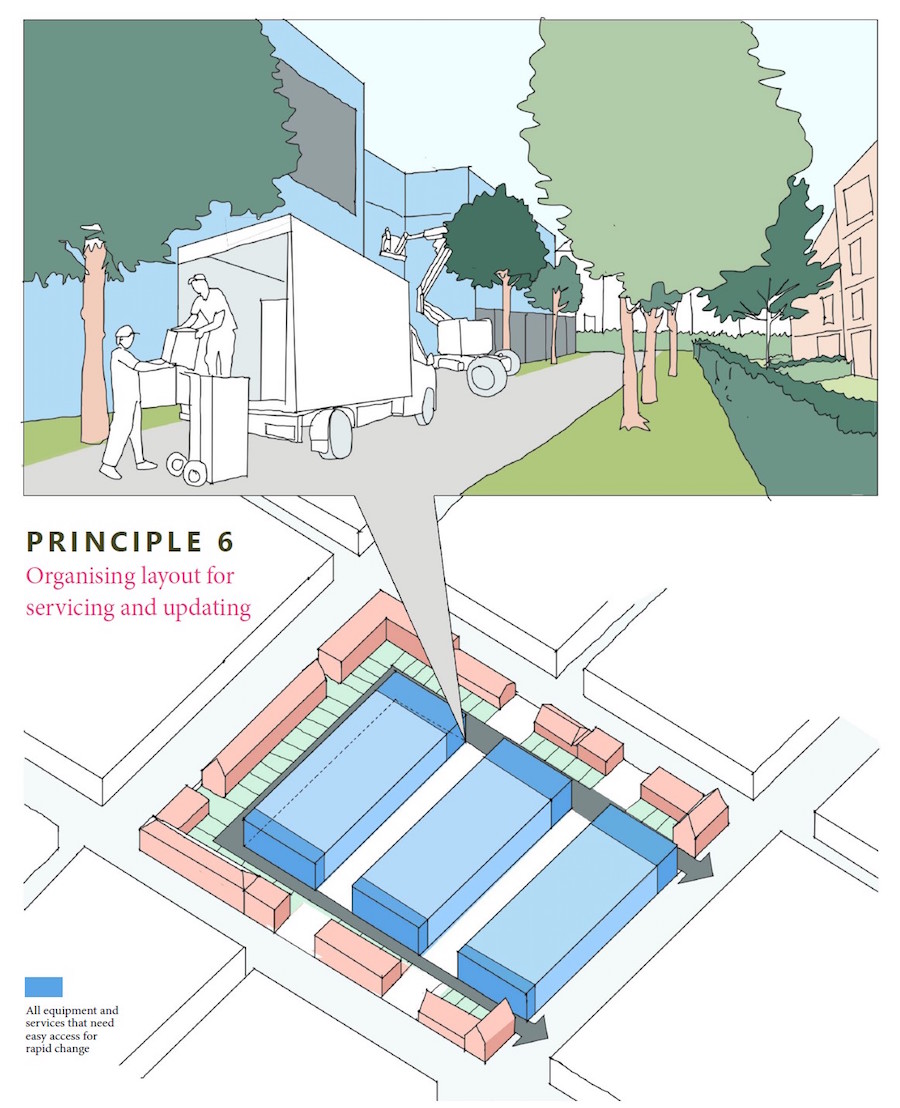
The quality of clinical outcomes, patient experience and staff efficiency all depend partly on fast-changing technological innovation. Together with the facilities management department, handling deliveries and the hospital’s complex waste-disposal system, all equipment and services that need easy access for rapid change are located next to the hospital’s private access roads within the block. This generates our sixth principle: Organising layout for servicing and updating (see Fig.11).
Hospitals have complex internal circulation requirements. People are there for very different reasons: some work there every day; others are unfamiliar with the place; and many are very stressed. Legibility and psychological atmosphere are key design considerations23.
The overall aim of the system is to provide privacy and dignity for patients, together with easy horizontal and vertical access between departments, separately for staff and for visitors. To make this work, we organise separate main systems of horizontal and vertical access for staff and for visitors, giving access to opposite ends of a central zone of clinical spaces for diagnosis, treatment and rehabilitation, which are located between the green corridors. Each of these clinical zones then has its own internal circulation, linking between the main staff and visitor systems.
The main staff system, frequently used to move between departments, gives rise to many unplanned encounters between staff members. Research suggests that these offer opportunities for impromptu discussions that are important for the effectiveness of the system overall24,25. We therefore design them with subspaces to facilitate these moments of ‘serendipity’.
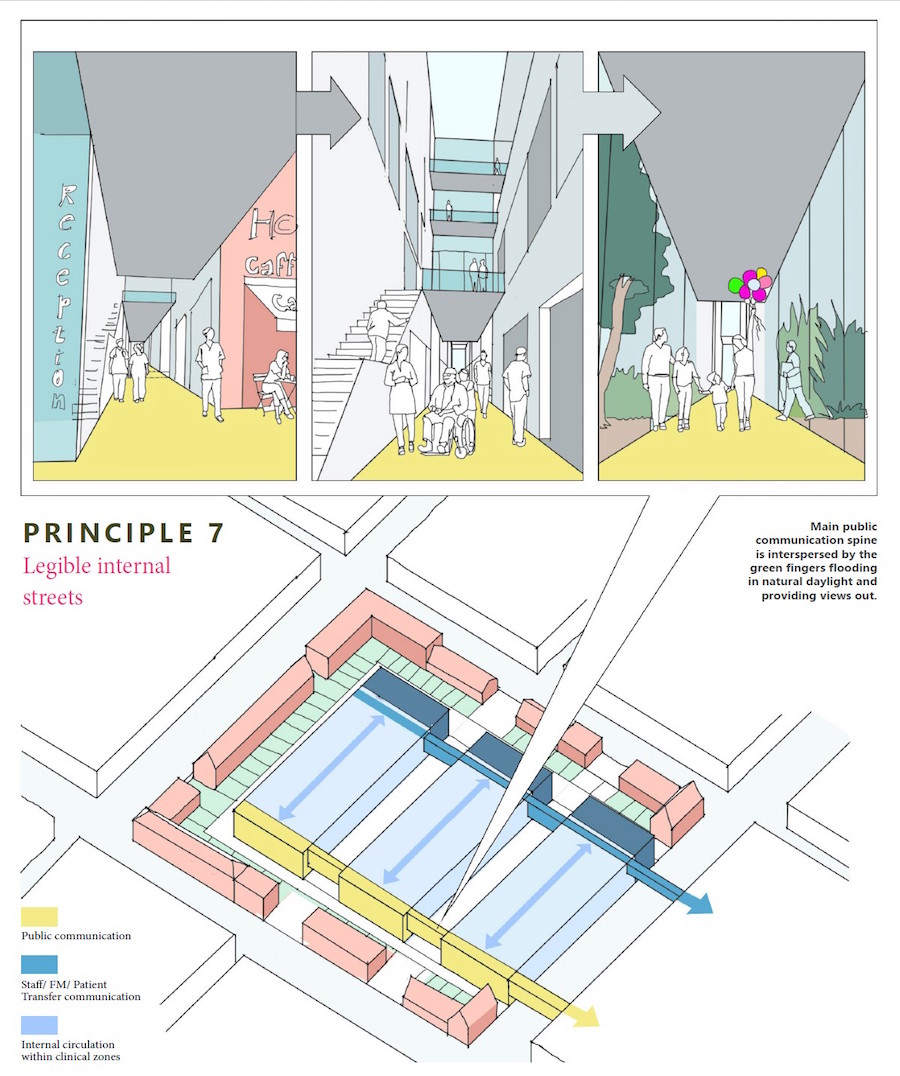
The main public system is used by people who are often highly stressed and anxious. As well as being directly legible, therefore, they offer a sequence of sensory experiences designed to create a low-stress balance between boredom and over-stimulation. Here, too, we have subspaces that provide settings for reflection, somewhat out of the main flow. These considerations generate our next design principle: Legible internal streets (see Fig.12).
To benefit patient experiences, clinical outcomes and staff wellbeing, hospitals must be able to adapt to changing health and care demands and technical services over time. As the move towards greater distribution of services within the region gathers pace, the balance of space requirements between hospital facilities and related housing and other services is likely to change from time to time.
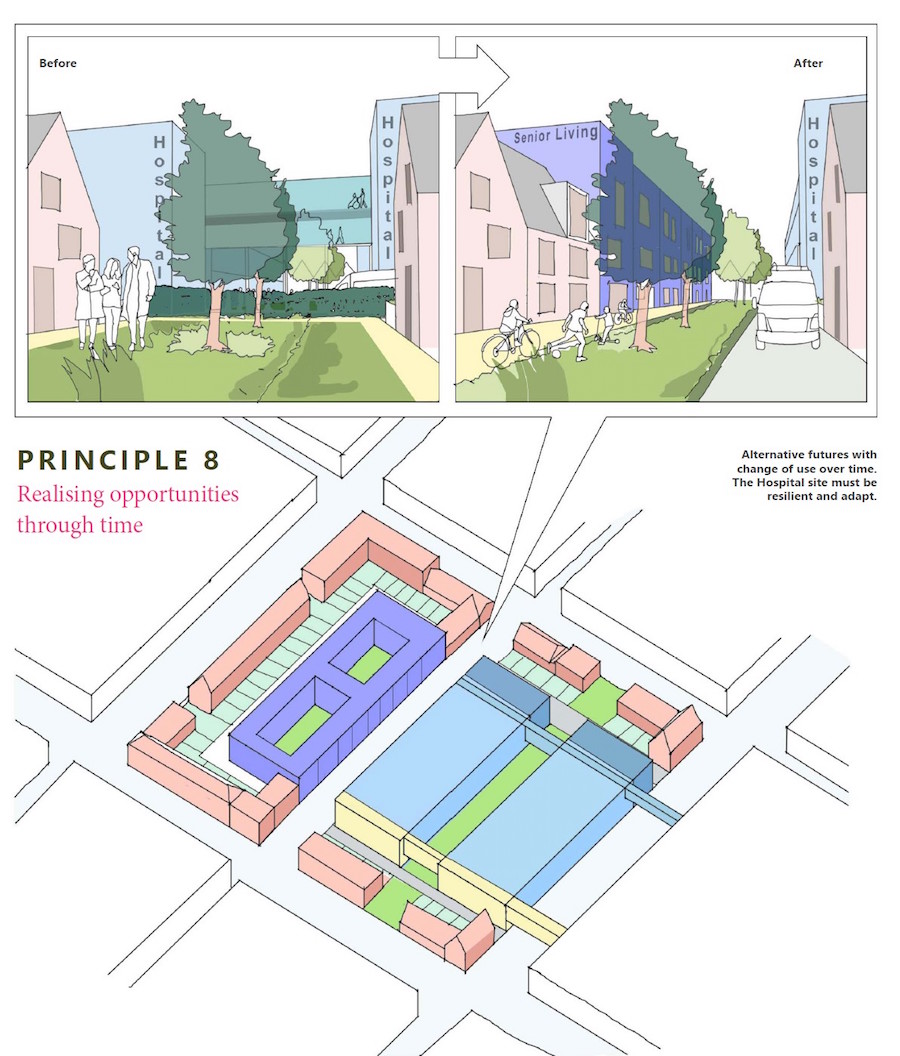
Our typology allows NHS real estate to stay connected with opportunities as they evolve. At the block scale, green courtyards can become new green streets, allowing hospital elements to accommodate more outward-looking activities such as housing, teaching or research facilities. This generates our eighth principle: Realising opportunities through time (see Fig.13).
The building scale
This adaptability is reinforced through design at smaller scales. Historically, the NHS has developed, with varying degrees of application and success, a standardised approach to the healthcare estate based largely on template designs. In more recent times, particularly with the Private Finance Initiative programme, hospitals have been designed as non-standard bespoke buildings, which have subsequently proved difficult and costly to change26.
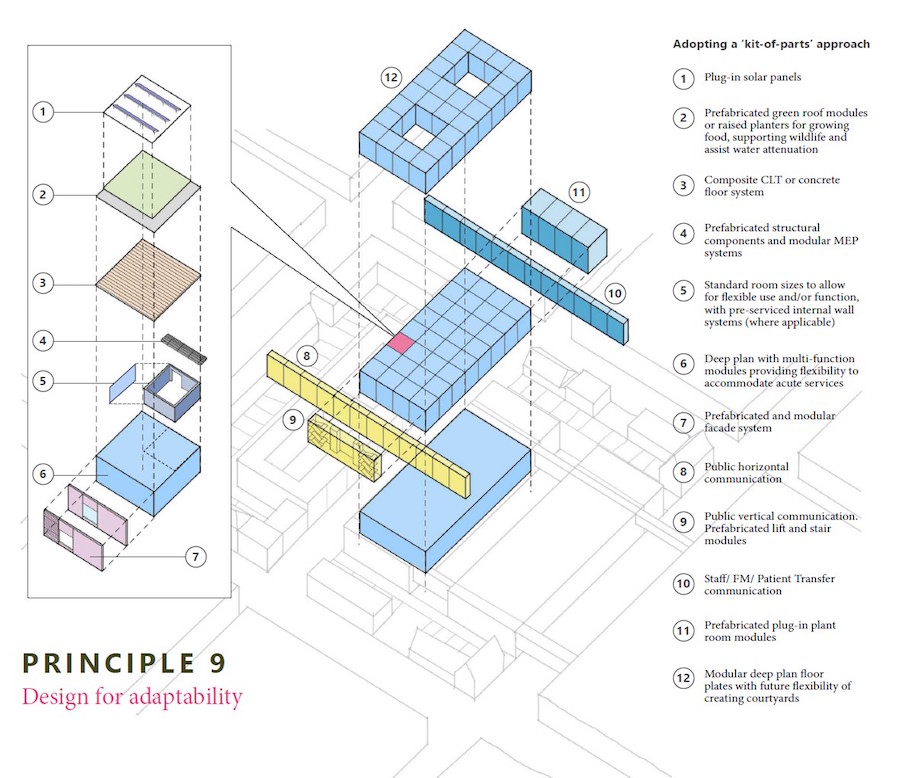
Recent developments in building and engineering systems, manufactured off-site in controlled factory settings, now offer the possibility of developing a more flexible and adaptable approach to the design of hospitals and other related facilities27. Modern methods of construction (MMC) offer the possibility of developing a hospital standard ‘kit of parts’, manufactured to the specific quality standards required by the NHS. Dimensionally, the kit of parts will be based on the planning grid for a ‘standard room’, sized to accommodate a range of common functions, ranging from inpatient room through consulting and examination room, treatment room, utility room, staff base, and so on. This average room size28 has the potential for creating standardised settings for common procedures, with consequent training advantages. The average size will be multiplied to provide for the variety of larger sizes that hospitals often require, and it will also inform the structural grid and associated sizes of all structural components. This generates our ninth principle: Design for adaptability (see Fig.14).
Conclusion
Ultimately, a hospital’s performance is built on the underlying health of the population it serves. We therefore need planning and design principles across a range of spatial scales, which enable hospitals to treat illness in ways that also support the building of underlying wellness.
 At the regional scale, our ideas build on the NHS drive towards geographically based integrated care systems. Learning from international precedents, we propose distributing the facilities of each integrated system throughout its region, in relation to its population’s spatial demographics, through a range of health hubs and campuses.
At the regional scale, our ideas build on the NHS drive towards geographically based integrated care systems. Learning from international precedents, we propose distributing the facilities of each integrated system throughout its region, in relation to its population’s spatial demographics, through a range of health hubs and campuses.
At the scale of the particular hub or campus, our principles reimagine hospitals as the seeds of neighbourhoods that foster wellness by supporting active lifestyles. Creating links between the hospital and the neighbourhood’s wider activities, these ideas also have implications enhancing the value of the NHS real estate, potentially increasing the funding available for the hospital facilities themselves.
Finally, at the smallest scale, we have developed design ideas for the spatial structure and physical construction of the hospital elements themselves. Here, we have focused on improving patient experiences, clinical outcomes, staff wellbeing, and integration with wider health and social care at the most personal level.
Taken together, the principles we have developed should not be seen as a rigid recipe. Focused on creating positive relationships between the potentials of particular regions, neighbourhood contexts and healthcare demands, their outcomes will depend on the nature of these potentials in each particular location. If used creatively, therefore, the same underlying principles will always generate situation-specific outcomes. There is, however, a common factor: these principles help the designer break free from the conception of the hospital as an isolated element (see Fig.15). The whole, in healthcare terms, becomes more than the sum of its parts.
About the authors
Prachi Rampuria and Soham De are co-founder directors of EcoResponsive Environments, a multidisciplinary practice working across urban design, architecture and art. Danny Gibson and Kieren Morgan are both directors and principal consultants at MJ Medical, a leading healthcare planning and design consultancy.
References
- BBC News. (2021). 11 charts on the problems facing the NHS. [online] Available at: https://www.bbc.co.uk/news/health-50290033 [Accessed 10 June 2021].
- Publications.parliament.uk. (2021). House of Lords. The Long-term Sustainability of the NHS and Adult Social Care, Select Committee on the Long-term Sustainability of the NHS. [online]. Available at: https:// publications.parliament.uk/pa/ld201617/ldselect/ldnhssus/151/15106.htm [Accessed 10 June 2021].
- Muller, W. (2001). Order and Meaning in Design. Utrecht: LEMMA, p.13.
- Raworth, K. (2017). Doughnut Economics: Seven Ways to Think Like a 21st-Century Economist, Vermont USA: Chelsea Green Publishing.
- World Health Organization. (2001). ‘Innovative care for chronic conditions: building blocks for action’, Global Report, p6. Available at: https://www.who.int/chp/knowledge/publications/icccglobalreport.pdf
- NHS. (2019). Long Term Plan. Available at: https://www.longtermplan.nhs.uk
- Bracebridge. (2017). Muskoka and Area Health System Transformation, ‘General Committee Agenda’, p.4. Available at: https://bracebridge.civicweb.net/document/18095
- Wang, Xin, et al. (2018). ‘The Luohu Model: A template for integrated urban healthcare systems in China’. International Journal of Integrated Care, 18 (4): 3, p.4. Available at: https://doi.org/10.5334/ijic.3955
- Goodwin, N, et al. (2017). Handbook Integrated Care, Oxford: Springer International Publishing, pp.3-4.
- NHS. Digital Transformation. Available at: https://www.england.nhs.uk/digitaltechnology/
- Lambert, V. Inside the hospital of the future. Available at: www.telegraph.co.uk/wellbeing/future-health/hospitals-of-the-future/ [Accessed 15 June 2021].
- Sevtsuk, A, et al. (2016). Pedestrian accessibility in grid layouts: The role of block, plot, and street dimensions. In Urban Morphology, 20 (2): 89-106.
- Gehl, J. (2010). Cities for People, Washington: Island Press, Chapter 2: Senses and Scale.
- March, L, and Steadman, P. (2020; First edition: 1971). The Geometry of Environment; and Berghauser-Pont, M, and Haupt, P. (2007). The relation between urban form and density. In Urban Morphology, 11 (1): 62-65.
- Bentley, I, et al. (1985). Responsive environments: A manual for designers, London: Architectural Press.
- Ulrich, RS. (1984). ‘View through a window may influence recovery from surgery’. In Science, Issue 4647: 420-421.
- Wilson, EO. (1985). Biophilia, Cambridge, Mass: Harvard University Press.
- Gidlow, CJ, et al. (2016). ‘Natural environments and chronic stress measured by hair cortisol’. In Landscape and Urban Planning, 148: 61-67.
- Sullivan, WC, et al. (2004). ‘The fruit of urban nature: Vital neighbourhood space’. In Environment and Behavior, 36 (5): 678-700.
- Forman, RTT. (1995). Land mosaics: The ecology of landscapes and regions, Cambridge: Cambridge University Press.
- Brand, C, and Hunt, A. (2018). The health costs of air pollution from cars and vans. 10.13140/RG.2.2.25409.86886.
- Assets.publishing.service.gov.uk. (2021). [online]. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/957205/National_Model_Design_Code.pdf [Accessed 18 June 2021].
- Yang, H. (2021). Emotional Journey | Service Design Tools. [online]. Available at: https://servicedesigntools.org/tools/emotional-journey [Accessed 15 June 2021].
- Hertzberger, H. (2015). Architecture and Structuralism: The Ordering of Space, Rotterdam: NAI, p.80.
- Carthey, J. (2008). Reinterpreting the hospital corridor: “Wasted space” or essential for quality multidisciplinary clinical care? HERD: Health Environments Research & Design Journal, 2(1), pp.17-29.
- Burke, A. (2014). Towards a new hospital architecture. University of East London, pp.39-40. Available at: https://repository.uel.974d10d07d3aa187dbd7b426c64fdba76af39fcf78a049c/22109043/140314_Complete_PhD_FINAL%255B1%255D.pdf [Accessed 15 June 2021].
- Roots Analysis. (2021). ‘Modular facilities in pharmaceutical and biotechnology market (2nd edition) …’. Available at: https://www.rootsanalysis.com/reports/view_document/modular-facilities-inpharmaceutical-and-biotechnology-market-2021-2030/178.html [Accessed 15 June 2021].
- Olsson, N and Hansen, G. (2010). Identification of critical factors affecting flexibility in hospital construction projects. HERD: Health Environments Research & Design Journal, 3(2), pp.30-47.
Organisations involved



