Healthcare / Net zero
Healthy hospitals for a healthy planet: Balancing carbon versus space
By Gavin Crook and Anuradha Sabherwal | 21 Dec 2023 | 0
The National Health Service’s Net Zero Building Standard sets a precedent for healthcare providers worldwide to take proactive steps to mitigate climate change. It became compulsory for all future NHS new building projects and refurbishments in October 2023. Here, Gavin Crook and Anuradha Sabherwal share what this vital but challenging new standard means for the industry – and why a delicate balance must be struck between minimising carbon and maximising space.
Authors of scientific paper:
Abstract
The mandate to design all new NHS buildings as net-zero carbon (NZC) is undoubtedly right, but progress in tackling the climate emergency is uncomfortably slow. Hospitals use a lot of energy and therefore emit a lot of carbon. They run 24 hours a day, 365 days a year, and must be kept running without reproach.
Most large acute city centre hospitals will not achieve the true definition of carbon zero – where the energy needed to function (operational) is met by technology, such as photovoltaics, wind turbines or fuel cells, with no harmful emissions. Worse still, the vast amounts of carbon necessary to build new facilities (embodied) also need compensation.
Newly released carbon emission thresholds will impact how we design and build hospitals. Even after implementing innovative architectural designs, applying efficient systems, and constructing in the cleanest way, most new hospitals will rely on financial offsetting. So how can we make the most efficient use of the NHS’s limited resources to help mitigate the climate crisis and move away from a reliance on carbon offsetting?
The energy and carbon targets for creating NZC hospitals are achievable through well-tested, new technologies, such as an all-electric energy system, a high-performance, climate-sensitive envelope, and efficient space planning. But it all comes at the cost of space. To hit these targets, in addition to infection control concerns, hospital ventilation systems must be more efficient. The only solution seems to be making everything larger – plant rooms, risers, and ceiling voids.
This significantly impacts demand for services space, which will need to be compensated by reducing clinical space within a fixed building volume – meaning fewer bedrooms, consultation rooms and theatres.
This presentation will discuss two important hospital schemes where we’ve explored innovative ideas and solutions that can help achieve a NZC healthcare building design. We’ll present the challenges and impacts of NZC on designing healthcare spaces through a case study on the Cambridge Cancer Research Hospital. We’ll focus on the design opportunities within the constraints to find the right design solutions, including adopting new technologies for a climate-positive hospital building.
Keywords
In February 2023, the UK’s National Health Service (NHS) issued the UK’s first Net Zero Building Standard for delivering net-zero carbon healthcare buildings. In doing so, it created a blueprint – and set a challenge – for healthcare providers worldwide to follow.
The Standard is part of the NHS’s commitment to become net-zero by 2045 – a mammoth task it must be said. The NHS is the largest public-sector employer in the UK and responsible for meeting the healthcare needs of the UK population; more than 3000 buildings fall under its stewardship, contributing 4-5 per cent of the UK’s total carbon emissions each year.
Why now?
The NHS’s decision to become the first health system to embed a net-zero target into legislation (via the Health and Care Act 2022) is bold and takes a proactive approach towards mitigating climate change. With the performance and priorities of the NHS under constant scrutiny, it could be argued that funds are better invested in boosting patients’ clinical services than decarbonisation. However, we believe that decarbonisation is healthcare, and that failing to act will cost far more in the long run. Climate change-related health problems are rising, laying an added burden onto an NHS already under deep strain.
A King’s College London study1 of nine English cities found that on high-pollution days, there are 673 additional out-of-hospital cardiac arrests and hospital admissions for stroke and asthma, with a spike in ambulance call-outs. For asthma alone, best estimates suggest more than one-third of new cases could be avoided by cutting carbon emissions.
The impact of rising temperatures has already proved vastly expensive to manage. The Royal College of Physicians reported that the 2003 heatwave cost the NHS £41.4 million2. The NHS spends over £50 million a year on carbon permits3 to offset its CO2 production. Indeed, climate change threatens the viability of the NHS, such that the UK Government has described climate change as “the most important health threat of the century”.
The costs of failing to decarbonise one of the UK’s biggest institutions are now simply too high from myriad perspectives: legal, financial, social and health.
Why develop a standard for new buildings?
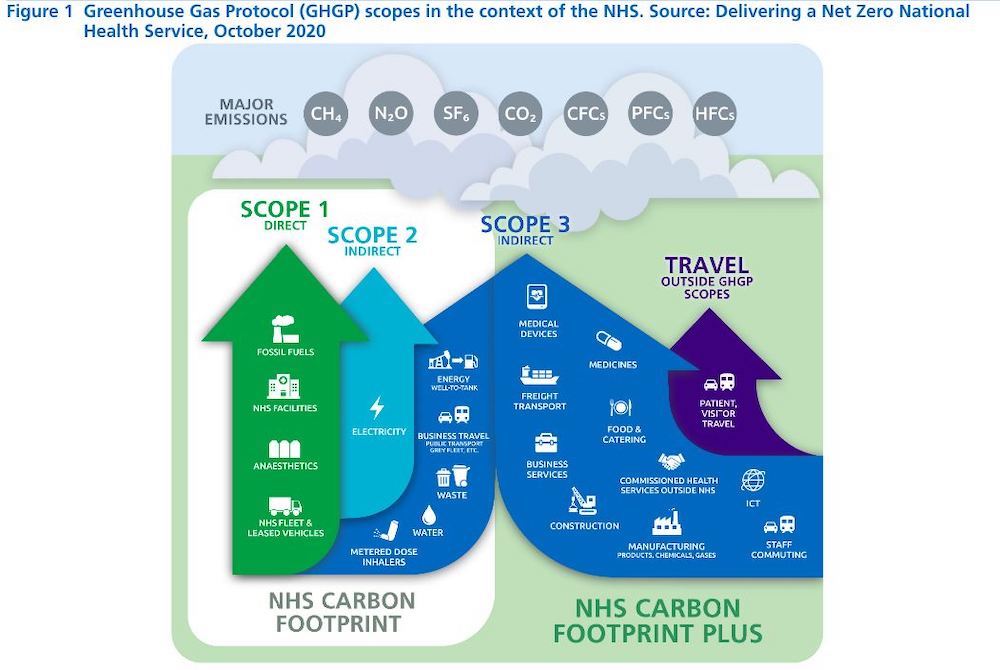
Healthcare buildings are energy and resource-hungry spaces, running 24/7 throughout the year. Decarbonising new buildings can only shave a small slice off the NHS’s total carbon emissions. Much more work is needed to reduce carbon and energy used by existing building stock; NHS scope 1, 2, 3 and travel emissions.
By making it mandatory for new buildings to be net-zero carbon, the NHS is setting a strong precedent and pathway for future carbon reduction efforts through implementing incremental innovations and technologies. In time, as the NHS estate decarbonises and older buildings are decommissioned, a more efficient estate will be created. As one of the largest employers in the world leading by example, the NHS also can influence other major global public health institutions to follow suit.
Developed with healthcare, industry and sustainability partners in committing to becoming net zero by 2045, the NHS has aligned itself with the UK’s broader, legally binding Net Zero 2050 targets and international efforts to mitigate climate change.
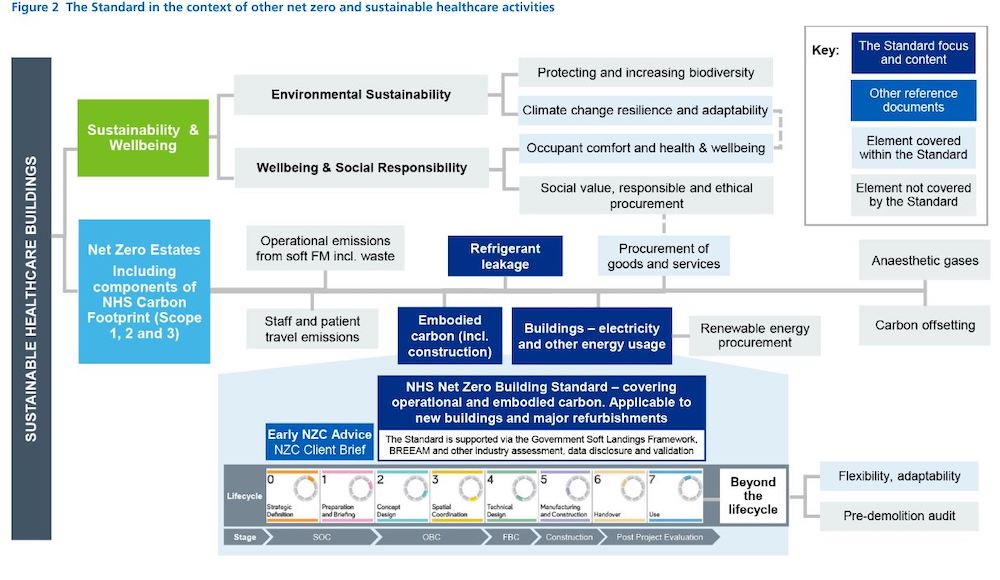
The Standard applies to all investments in new buildings and major upgrades to existing facilities from October 2023, providing technical guidance to develop sustainable, resilient and energy-efficient healthcare buildings.
How can it be achieved?
The Standard sets out an approach to low-carbon building design by setting performance criteria for key design drivers that include:
- minimum performance targets (MPTs) for construction U-values and building services plant efficiencies;
- setting carbon limits for operational energy on a departmental basis and embodied carbon for the major components of the building; and
- crucially requiring reporting of whole-life carbon – both to create an accurate picture of the carbon output of a building and to inform and refine future iterations of the Standard.
The challenges: Applying the NHS Standard to our hospital designs
Creating a sustainability standard for inherently energy-intensive buildings is immensely difficult, not least when it must be integrated alongside other best practice guidance for achieving high-quality healthy, sustainable buildings.
The Standard is inherently adaptable and recognises hospitals’ high base energy demand and the importance of health and wellbeing to support a more holistic approach to sustainability. It’s the first UK publication that defines a methodology to start decarbonising the multi-billion-pound physical estate. The methodology will undoubtedly need to improve with time, as learnings from different hospital cohort groups are made available. It’s evolving and being actively tested via our projects.
Making space
The energy and carbon targets for creating net-zero carbon hospitals are admirably low, achievable through well-tested, robust and reliable new technologies, such as an all-electric energy system, fossil fuel-free energy supplies, a high-performance climate-sensitive building envelope, and efficient space planning. But it comes with a cost: clinical space.
To hit these targets, in addition to infection control concerns, hospital ventilation systems must become more efficient. Owing to the uncompromising laws of physics, the only solution seems to be making everything larger – plant rooms, risers, and ceiling voids. This significantly impacts the demand for services space, which will need to be compensated by either reducing clinical space within a fixed building volume, potentially meaning fewer bedrooms, consultation rooms, and theatres. Alternatively, it may imply increasing the overall volume of space and associated costs.
Our biggest challenge as designers is creating that balance between ensuring we achieve sustainability goals within the NHS's project budgets without impacting the critical clinical delivery pathways and outcomes within the flexibility needed for future change.
An adaptable hospital
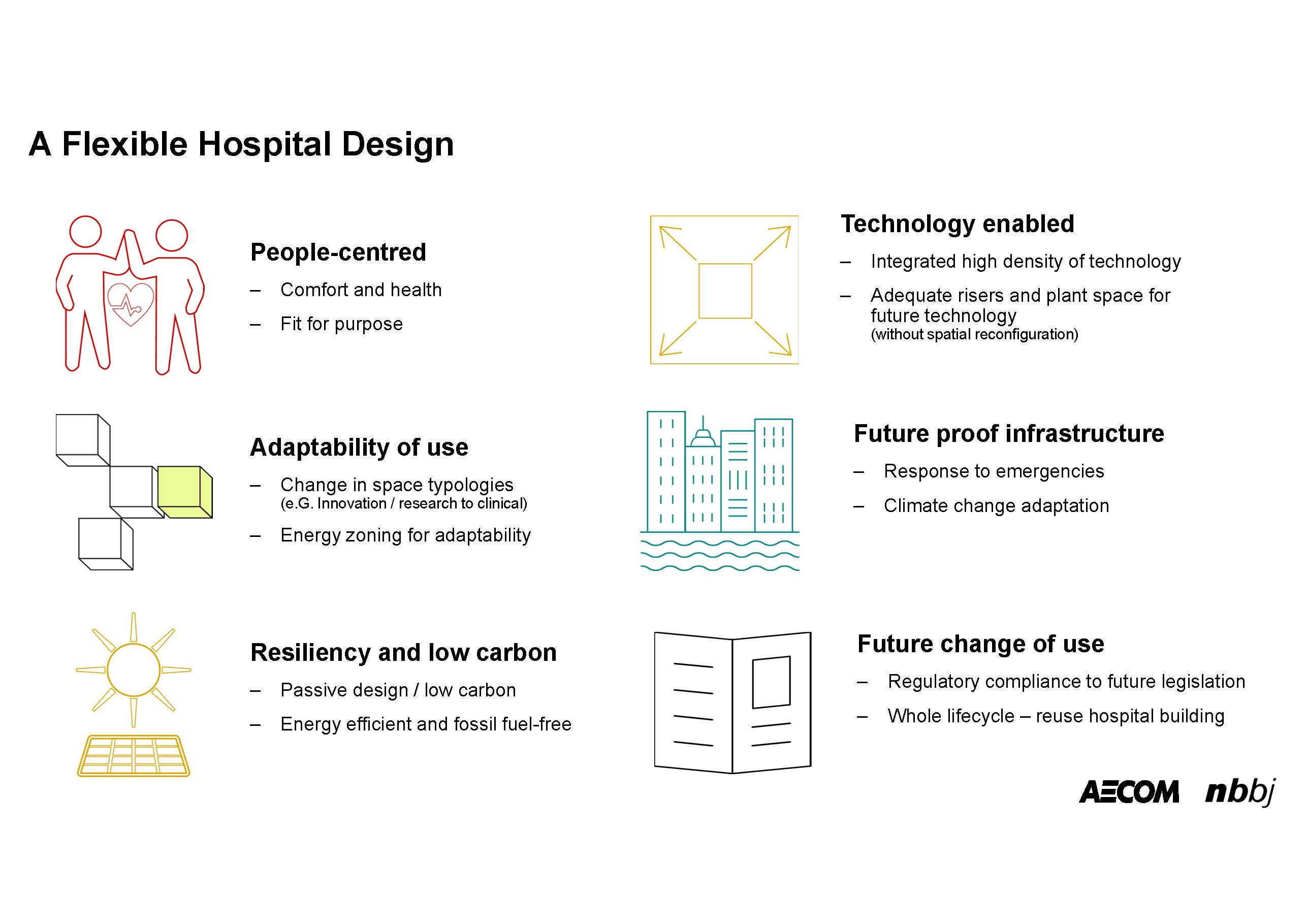
An adaptable hospital would foresee the need to accommodate changes in the use of spaces in how the services and systems are designed. As designers, we always incorporate elements of this into healthcare design. However, under the spotlight of carbon neutrality, more thought needs to be given to true flexibility, as it can have a noticeable effect on the day-one design.
The advantage of a flexible hospital will be a longer-term reuse capability avoiding the implications of (at worst) demolition and rebuilding, which has substantial embodied carbon cost. A fully flexible hospital would incorporate everything at day zero that could be needed in the future, avoiding the capital carbon costs and waste generated through rebuilding. Systems could be designed with in-built redundancy, spare capacity, and physical space so that the building can adapt and flex as future needs evolve.
The design of resilient and sustainable healthcare buildings must be able to adapt to future change to be relevant and low-carbon, taking a whole life-cycle approach. The fundamental design elements of a hospital that lend themselves to integrating future change are:
- People-centred design: Hospitals prioritise patient comfort, safety and wellbeing. People-centred design focuses on creating environments that promote healing, privacy and positive experiences for all. Integrating passive design within hospital buildings enables naturally lit, comfortable and welcoming spaces that support health and opportunities for social interaction, which can be adaptable to other uses; it also provides the biggest savings in energy and carbon at very early design stages by reducing the operational carbon footprint.
- Sustainability and resiliency: Hospitals already embraced sustainable design principles to reduce environmental impact and operating costs. They operate continuously for long periods and can justify investment in energy-efficient systems based on heat recovery, fossil-fuel free and renewable energy sources, water conservation measures, and waste management strategies.
- Technology integration: Hospitals integrate advanced technologies that support effective healthcare delivery, and they can easily allow a high density of other IT systems. Providing adequate service riser and plant spaces from the beginning, and factoring these in early in the cost plan, will enable the hospital to integrate future technologies without the need to reconfigure space.
- Future-proof infrastructure: Hospitals have robust infrastructure, including reliable electrical systems, data connectivity, and backup power sources. This infrastructure should be designed as scalable and adaptable to accommodate future technology upgrades and expansions. Additionally, hospitals must consider resiliency features to withstand disasters and ensure continuous operations during emergencies.
- Clinical delivery, research and innovation spaces: Hospitals provide dedicated spaces for translational research, innovation, and education, fostering collaboration with clinical delivery methods among researchers, clinicians and industry partners. Designing space typologies tailored to their specific functions and energy use intensity is key to controlling both regulated and unregulated loads. Zoning spaces and services is key to achieving this flex in the adaptability of one part of the hospital function to change use, for example, from low-tech space such as a clinical outpatient unit to a high-tech research space, such as a clinical trials laboratory.
- Regulatory compliance and future standards: Hospitals must stay informed about evolving healthcare regulations, guidelines and standards. Designing and constructing hospitals with future regulations and requirements in mind will ensure long-term compliance and reduces the need for costly retrofits or renovations.
Testing the implications of the Standard
We’re testing the implications of net-zero design on live projects, including the Cambridge Cancer Research Hospital.
Cambridge Cancer Research Hospital
The new Cambridge Cancer Research Hospital (CCRH) is a collaboration between Cambridge University Hospitals NHS Foundation Trust, the University of Cambridge, Cancer Research UK, and commercial partners. The 27,083m² project is a standalone building with seven floors plus a small basement. It houses inpatient bedrooms, day cancer treatment, alongside a dedicated diagnostics/imaging department, a cancer assessment unit, outpatient clinics, and various research labs, with underground links to the adjacent main Addenbrooke’s Hospital for transfer of patients and FM services.
Due for completion in 2028, the hospital will be a key centre of care and translational research for cancer patients and an early example of the NHS’s net-zero carbon building standard in practice. The average hospital on the Addenbrooke’s Hospital campus uses around 405-470kWh/m2 of operational energy a year; the CCRH’s operational energy target will be more than half this consumption, at 200kWh/m2 a year through a number of incremental savings in design measures.
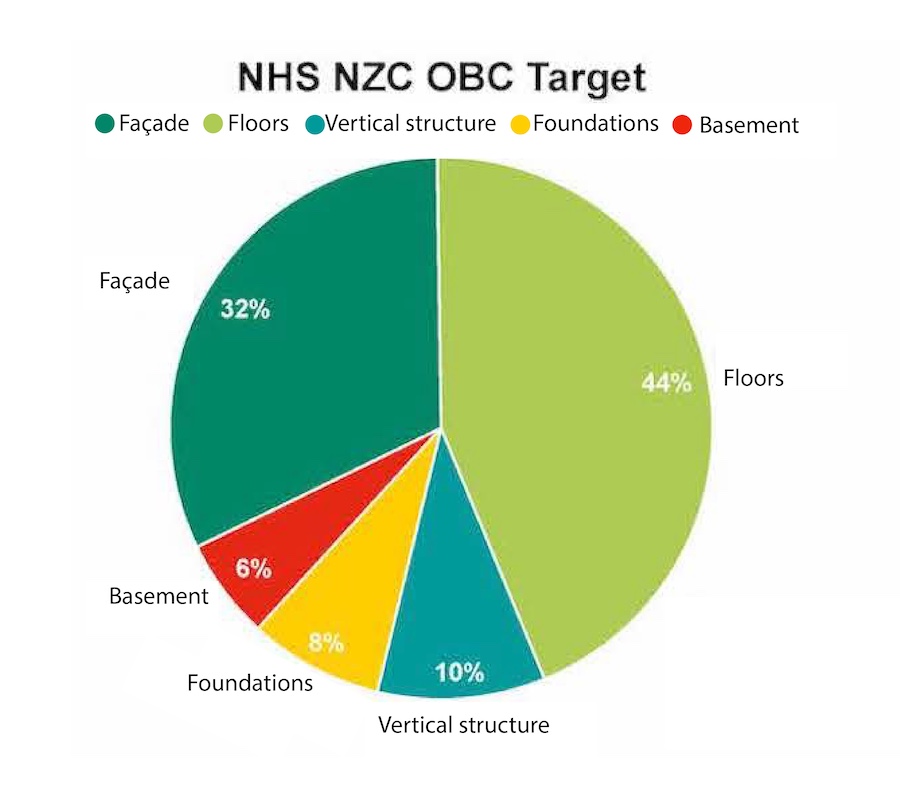
It also sets a methodology and carbon factors to estimate the embodied carbon of the facade, superstructure and sub-structure, estimated to contribute around 65-70 per cent of the total embodied carbon of the building.
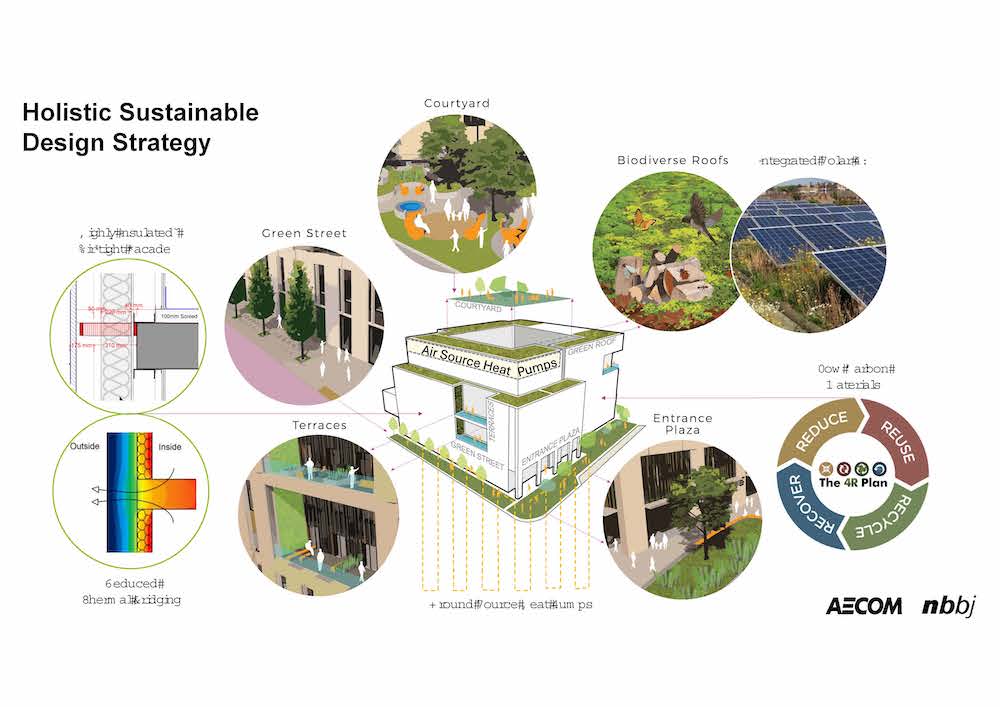
The Standard focuses on energy intensity of spaces, which forms the crux of the decarbonisation challenge for hospitals, because the energy needs of different hospital departments vary significantly. Our approach has differentiated the design between high-, medium-, low-tech, and ultra-high support in accordance with the NHS Standard. To achieve the ambitious carbon reduction target for the CCRH, we’re focusing on the following:
- being lean – reducing energy demand through passive design measures and optimising clinical space design;
- improving fabric – designing a highly insulated, high-performance building envelope;
- decentralised plant – minimising service runs and providing plant space near the specific clinical functions;
- creating clean onsite energy – onsite solar photovoltaics on a biodiverse green/blue roof;
- efficient use and reuse of heat and cooling – through integrating air-source heat pump (ASHP) and ground-source heat (GSHP) technologies; and
- measuring through a whole life-cycle carbon approach.
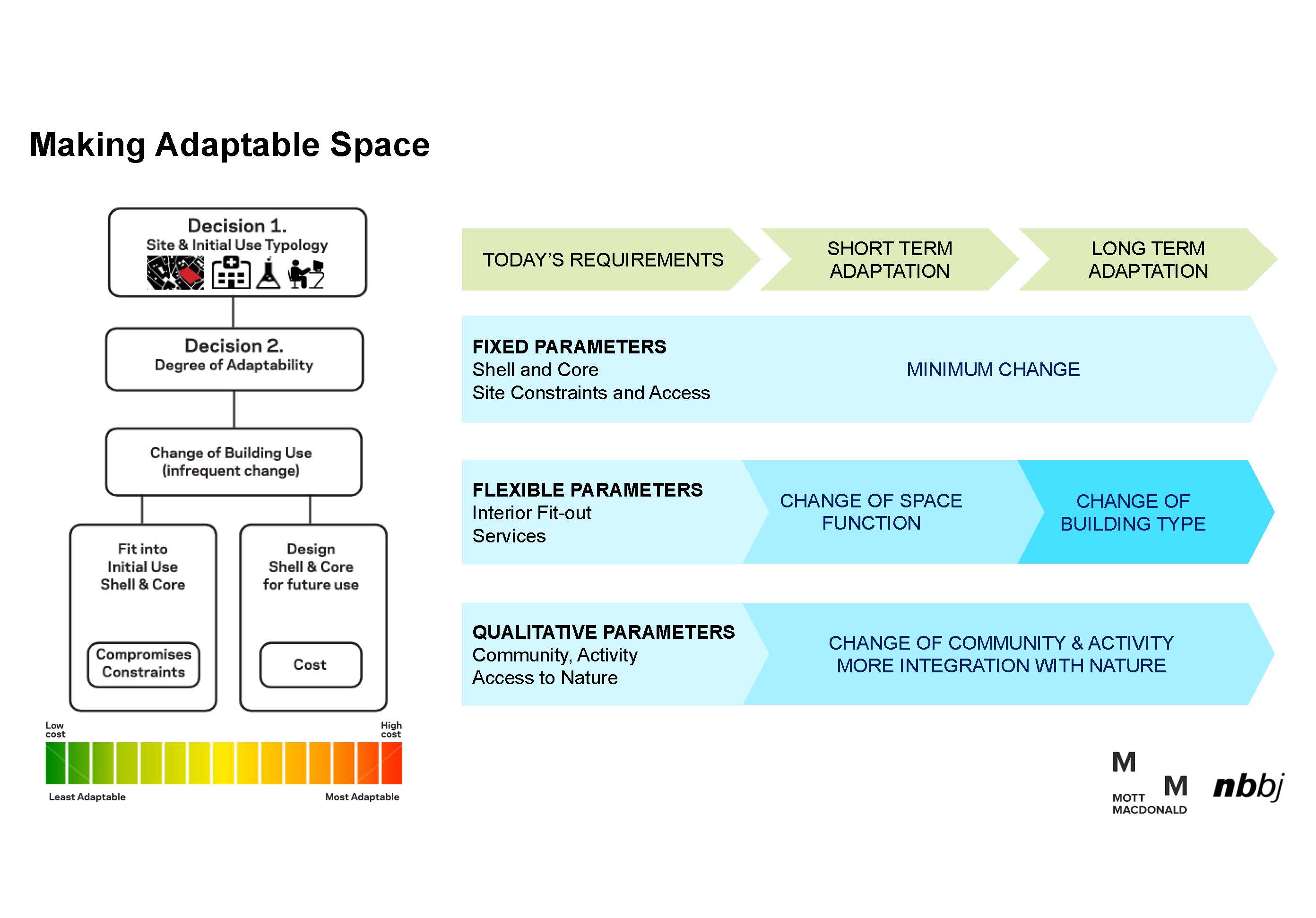
One of the key design drivers of the CCRH as a net-zero carbon hospital is the reuse or repurposing of the hospital for changes in functionality. We’ve optimised space and cut carbon by creating a highly flexible hospital floor plate that can increase the lifespan of the new building. This protects against future space redundancy by enabling change of use to respond to changing clinical cancer care delivery methods and allowing for new, better technologies to be integrated later.
The CCRH design is based on a highly flexible space planning approach. Its grid and structural design have been designed to accommodate loadings for different functions and future changes of use of hospital departments: for example, outpatient areas can be converted into future wards (or vice-versa) or laboratories as needed. With a flexible two-way flat concrete slab solution avoiding down-stand beams and utilising low carbon concrete additives, it also future-proofs changes in ceiling services with minimal constraints.
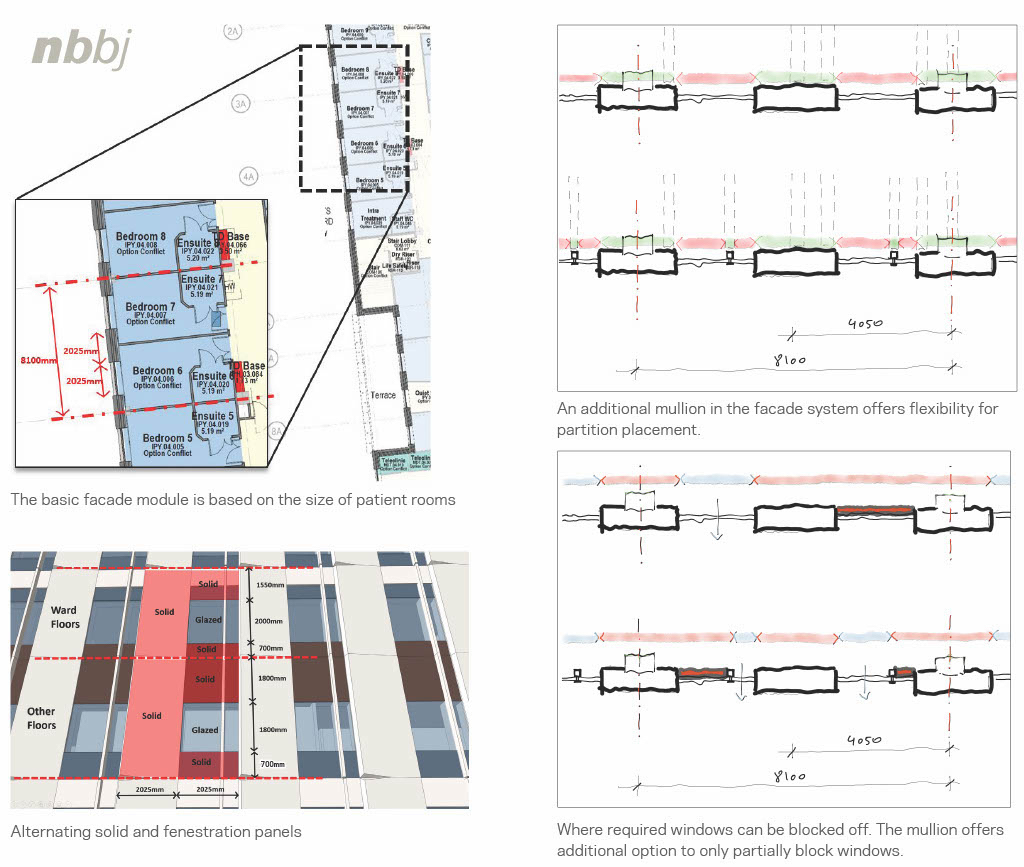
This need for flexibility also informed the facade strategy, where facade panels have been designed for offsite manufacture and follow the same grid modules as the interior spaces. Windows have been carefully sized to provide adequate daylighting without causing unnecessary overheating or heat loss that can increase the energy loads of the building. Flexibility in designed sill heights also enables different perimeter room layouts to adapt to changes in use without the need to alter the facade and windows.
The key to achieving the operational energy targets for the CCRH has proven to be the design of thermally high-performing, airtight facades, with more than 42-per-cent improvement of U-values compared with current Building Regulations Part L requirements. Along with a carefully controlled window-to-wall ratio of 20 per cent, the design mitigates against unwanted solar gain without compromising access to natural daylight and views out to roof gardens for supporting occupant health and wellbeing.
What have we learnt so far?
A key learning was the importance of clarity of brief and clear definition of sustainability benchmarks and targets. This enabled us to focus on designing flexibly and allowed the integration of decarbonisation strategies from the very beginning.
Detailed early embodied carbon reduction studies were critical to choosing the most suitable low-carbon structural system and materials with minimal cost impact. We also undertook early facade option studies to compare the embodied carbon of different systems, including rainscreen systems, precast concrete facades, and unitised facade systems, keeping the thermal performance requirement as the key constant.
Several aspects were considered while evaluating the choice of both structural systems and facades. These included offsite manufacturing potential, thermal performance efficiency, embodied carbon and weight of the structure, and facades that, in turn, impacted the embodied carbon of the structural frame and foundation design. Further carbon reductions have been achieved through the integration of onsite renewables.
We also found some constraints in designing hospitals as low-carbon, energy-efficient buildings, owing to limitations of the NHS Health Technical Memorandum guidance, which went against the implementation of passive design and low-carbon technologies. During the Covid-19 pandemic, for example, there was a strong emphasis on providing natural ventilation as a key health benefit. NHS guidelines, however, limit the use of natural ventilation because of the high levels of air exchange required in these spaces.
Natural ventilation also hinders the effectiveness of heat recovery and heat-exchanging technologies required to achieve energy efficiencies towards net-zero carbon design. Owing to the more onerous requirements of the new Building Regulations Part L, we found that ventilation loads were the highest, even though our design significantly reduced the heating and cooling loads. This brought us very close to achieving compliance with Building Regulations approvals, and we’re continuing to investigate to further improve and refine the design and Building Regulations compliance energy modelling.

Developing a clear methodology towards net-zero carbon design
To achieve the NHS and UK net-zero carbon ambitions, establishing a clear and holistic approach towards sustainable buildings design is crucial to ensure our design can achieve the balance required between upfront capital carbon and offsetting through onsite renewable energy generation, end-of-life reuse and, finally, minimal offsetting to achieve a net-zero carbon design.
Carbon measurement at all design stages and information transparency are at the heart of all these efforts. Close collaboration between design and sustainability leads is key to undertaking whole-life carbon analysis based on actual environmental product declarations (EPDs) and carbon declarations to industry standards. Residual emissions must be offset responsibly using recognised frameworks with clearly defined environmental, social and governance (ESG) goals to mitigate climate change.
After the building is operational, it’s important to refine and improve the building systems through energy monitoring and validate sustainability certifications through post-occupancy evaluations. At the end of the building’s useful life cycle, designs must integrate the potential to disassemble and reuse components to minimise waste, divert from landfills, and support a circular economy.
Our designs aim to set a benchmark of exemplar design for future hospitals that can enable NHS estates to transition to a low-carbon future and towards the overarching net-zero goals. We’ve fed back our learnings to further refine the NHS Standard by testing the benchmarks and methodologies. We’ve also engaged with the wider construction industry and its supply chain through detailed discussions and early engagement, sourcing low-carbon materials and pushing for greater information transparency.
One of our main challenges is that quality carbon data and information still needs to be improved within the industry. We hope that by sharing our learnings from our project experiences, we can engage with our peers to interrogate, research, and collectively develop a shared knowledge base and a whole life-cycle approach to realise the NHS’s net-zero carbon goals.
Conclusion
New healthcare buildings stand at the intersection between health, technology and design. With hospital buildings being vastly energy-intensive in their operation, construction and eventual decommissioning, creating a net-zero carbon hospital without financial carbon offsetting is unlikely to happen.
The NHS Net Zero Building Standard recognises this and aims to offset its overall carbon footprint at an institutional level rather than individual buildings. To reduce the reliance on carbon offsets to achieve our goals, we must make our designs as efficient as possible through incremental design solutions, so that carbon offsetting is minimised and only environmentally certified carbon offsetting schemes are supported. These may not be complete solutions yet, but they will create more efficient, less carbon-intensive methods of providing healthcare.
The NHS has already reduced its emissions by 30 per cent since 20104: this is just another step forward in making a low-carbon NHS a reality. The decarbonisation of NHS building design is a significant milestone in improving public health – and a great example of exactly why this institution was created.
About the authors
Gavin Crook is regional director, building engineering at AECOM and Anuradha Sabherwal is senior associate, sustainable design lead at NBBJ.
References
- Greener NHS campaign to tackle climate ‘health emergency’. (2020). NHS England. https://www.england.nhs.uk/2020/01/greener-nhs-campaign-to-tackle-climate-health-emergency/
- Breaking the fever: Sustainability and climate change in the NHS. (2017). Royal College of Physicians. http://www.rcplondon.ac.uk/projects/outputs/breaking-fever-sustainability-and-climate-change-nhs#:~:text=rcplondon.ac.uk-,Breaking%20the%20fever%3A%20Sustainability%20and%20climate%20change%20in%20the%20NHS,to%20reducing%20greenhouse%20gas%20emissions
- Sustainable services: Future trends. The King’s Fund. https://www.kingsfund.org.uk/projects/time-think-differently/trends-sustainable-services#:~:text=Carbon%20footprint%20of%20the%20NHS,set%20to%20increase%20over%20time
- ‘Healthier Planet, Healthier People’ staff engagement campaign. NHS England. https://www.england.nhs.uk/greenernhs/get-involved/staff-engagement-campaign/



